

A Long but Promising Stroke Recovery for Young, Healthy New Yorker
On December 13, 2019, 40-year-old Meaghan Onofrey was out for a run in Riverside Park. She remembers needing to suddenly stop, but after that, she has no recollection of the events that took place. According to her husband, Nick, she had collapsed and crawled to a bench, and a passerby called 911. Meaghan was taken in an ambulance to Mount Sinai Morningside, where tests were performed in the emergency room, and it was discovered that she was having a stroke. She was transferred to The Mount Sinai Hospital.
The diagnosis: a basilar artery occlusion caused a stroke in her brainstem and cerebellum. Meaghan underwent a thrombectomy—a minimally invasive endovascular procedure to remove the blood clot from the brain—and a decompressive craniotomy to reduce swelling, both performed by Tomoyoshi Shigematsu, MD, PhD, Assistant Professor of Neurosurgery, Neurology, and Radiology, Icahn School of Medicine at Mount Sinai.
“The quick thrombectomy saved her brainstem from a larger stroke, and the craniotomy saved her brainstem from compression,” Dr. Shigematsu says. “We were able to minimize the damage to the brainstem, although there is some damage causing weakness mostly in one side.”
Meaghan recovered in The Mount Sinai Hospital’s Neurosciences Intensive Care Unit for the next month. Although she was not conscious the entire time, Meaghan underwent scans and monitoring for intracranial pressure, and received a tracheostomy to enable her to breathe on her own. She was then discharged to inpatient rehabilitation. After a few weeks, fluid began developing around her brain—a condition known as hydrocephalus—and she underwent another procedure with Dr. Shigematsu to place a ventriculoperitoneal (VP) shunt in her brain to relieve pressure caused by the fluid. During her recovery from that surgery, she developed pneumonia and spent another month in the ICU, where she received a second tracheostomy, before going back to rehab.
By this time, the COVID-19 pandemic had reached New York City, and Mount Sinai began to restrict visitors to help limit the spread of the virus. That meant Nick could not visit Meaghan, which was difficult for her, but soon enough her unit was being transformed into a COVID ICU, and she was discharged home. To ensure their apartment was equipped with everything needed to help Meaghan recover, Mount Sinai staff assisted Nick with purchasing the proper medical equipment.
Throughout the pandemic, Meaghan received therapy via telehealth with occupational therapist Andrea Johnston; physical therapist Jeanette Mayr; and speech-language pathologists Carly Traiman and Brenda Lyons. She also saw a number of other specialists, such as an ENT physician, a gastroenterologist, and a neuro-ophthalmologist, some of whom she visited in person once outpatient offices opened up.
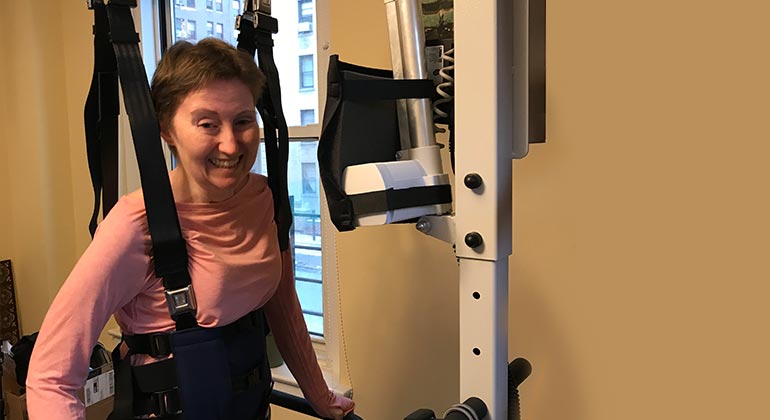
As of October 2020, Meaghan is able to stand with assistance, speak again, and eat almost everything, and is beginning to regain functionality in her right arm. She is also increasingly confident that she will be able to walk again, all thanks to the “top-notch” care she has been receiving at Mount Sinai. “It’s almost a year—I can’t believe it,” she says. “I can’t work, but I hope to be able to work someday. There’s a lot of stuff I can do. A lot has actually happened.”
Dr. Shigematsu is also pleased with Meaghan’s progress, “She and her husband worked together very hard and underwent very successful rehabilitation. I saw her recently, and I was amazed to see her excellent recovery.”
For Meaghan, there are two big takeaways from having a stroke. “It can happen to someone like me, who is very healthy. And the stroke journey is a long one—it takes a while. I’m pushing myself very hard and still, it takes a long time.”