Study shows medication-assisted treatment, including group therapy, improves the function of a brain area responsible for inhibitory control that is impaired in individuals with heroin use disorder

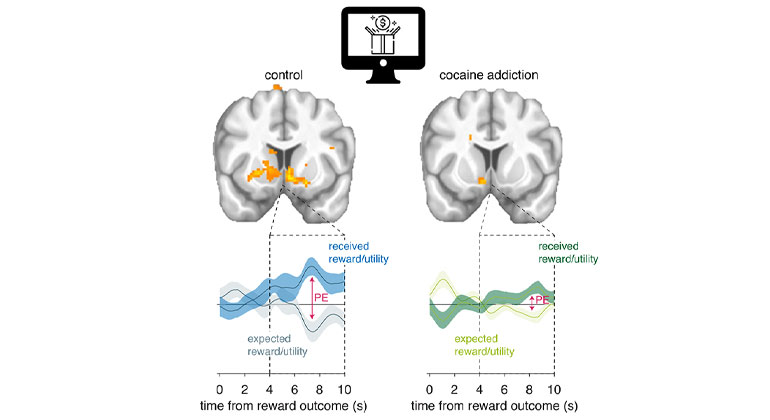
In line with their previous work, researchers from the Icahn School of Medicine at Mount Sinai showed that individuals with heroin use disorder have lower activity in the anterior and dorsolateral PFC when performing an inhibitory control task compared with healthy controls. Importantly, they revealed that 15 weeks of medication-assisted therapy, which included supplemental group therapy, improves impaired function of the anterior and dorsolateral PFC during an inhibitory control task among the group of participants with heroin use disorder, suggesting a time-dependent recovery of inhibitory control and PFC function in individuals with heroin use disorder after such a treatment intervention.
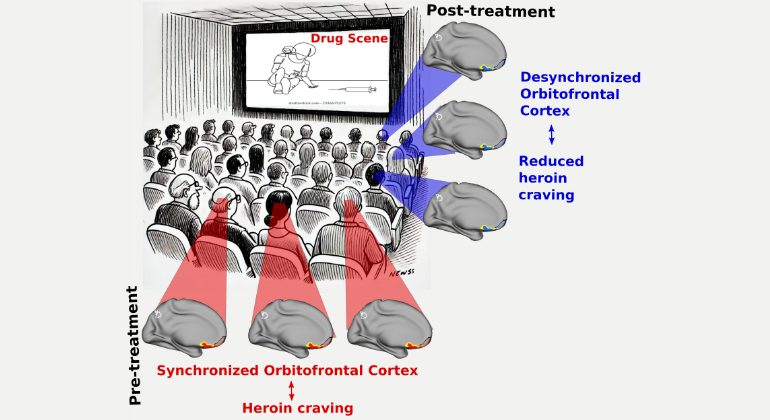
Opioid (including heroin) overdose-related deaths continue to increase at staggering rates among adults in the United States. Inhibitory control – the ability to suppress unwanted behaviors, such as drug use, despite substantial negative consequences and a desire to quit – is impaired in individuals with drug addiction and is accompanied by functional deactivations in the prefrontal cortex (PFC), a brain region that subserves self-control processes.
In this study, 26 inpatient individuals with heroin use disorder undergoing medication-assisted treatment and 24 demographically-matched healthy controls were recruited for a longitudinal task-based functional MRI (fMRI) study. Participants attended two fMRI sessions, separated by 15 weeks of medication-assisted inpatient treatment for individuals with heroin use disorder and a comparable time interval for healthy controls. During fMRI, the study participants performed a stop-signal task - a well-validated tool for estimating brain function during inhibitory control behavior. During the task, study participants responded to directional arrow stimuli and withheld their responses when the arrow occasionally turned red (the stop signal). In addition to showing increased activity in the PFC regions after 15 weeks of inpatient treatment, the increased activity correlated with better behavioral performance in the stop-signal task by individuals with heroin use disorder.
“Overall, our findings identify the anterior and dorsolateral PFC regions as potentially amenable to targeted interventions to potentially expedite their recovery during inhibitory control, which may have translational value to help inform future treatment methods,” says Ahmet O. Ceceli, PhD, senior postdoctoral fellow and lead author of the paper.
“More research is needed to determine if there is a specific aspect of inpatient treatment that substantially contributes to the improvement and to examine other specific factors. For example, our research team plans to test whether the recovery effects we observed in this study are attributable to the mindfulness-based intervention that was part of the supplemental group therapy intervention” says Rita Z. Goldstein, PhD, Professor of Psychiatry and Neuroscience at Icahn Mount Sinai and senior author of the paper.
About the Mount Sinai Health System
Mount Sinai Health System is one of the largest academic medical systems in the New York metro area, with 48,000 employees working across seven hospitals, more than 400 outpatient practices, more than 600 research and clinical labs, a school of nursing, and a leading school of medicine and graduate education. Mount Sinai advances health for all people, everywhere, by taking on the most complex health care challenges of our time—discovering and applying new scientific learning and knowledge; developing safer, more effective treatments; educating the next generation of medical leaders and innovators; and supporting local communities by delivering high-quality care to all who need it.
Through the integration of its hospitals, labs, and schools, Mount Sinai offers comprehensive health care solutions from birth through geriatrics, leveraging innovative approaches such as artificial intelligence and informatics while keeping patients’ medical and emotional needs at the center of all treatment. The Health System includes approximately 9,000 primary and specialty care physicians and 10 free-standing joint-venture centers throughout the five boroughs of New York City, Westchester, Long Island, and Florida. Hospitals within the System are consistently ranked by Newsweek’s® “The World’s Best Smart Hospitals, Best in State Hospitals, World Best Hospitals and Best Specialty Hospitals” and by U.S. News & World Report's® “Best Hospitals” and “Best Children’s Hospitals.” The Mount Sinai Hospital is on the U.S. News & World Report® “Best Hospitals” Honor Roll for 2025-2026.
For more information, visit https://www.mountsinai.org or find Mount Sinai on Facebook, Instagram, LinkedIn, X, and YouTube.