Mount Sinai Receives More Than $10 Million in Grant Funding for Brain Tumor Research
The Department of Neurosurgery at the Icahn School of Medicine at Mount Sinai has received more than $10 million in federal funding for several projects focusing on brain tumor research. The newest grant focuses on the use of magnetic hyperthermia therapy (MHT), a powerful nanotechnology-based treatment that may enhance the effects of radiation therapy and chemotherapy on glioblastoma tumors. The lead investigator is Constantinos Hadjipanayis, MD, PhD, Director of Neurosurgical Oncology at the Mount Sinai Health System and Chair of Neurosurgery at Mount Sinai-Union Square.
“Our neurosurgeons are at the forefront of clinical care and scientific research with the goal of translating research findings into new therapies that will improve patient outcomes,” said Joshua Bederson, MD, the Leonard I. Malis, MD / Corinne and Joseph Graber Professor of Neurosurgery at the Icahn School of Medicine at Mount Sinai, and Chair of Neurosurgery for the Mount Sinai Health System.
- Magnetic Hyperthermia Therapy for Glioblastoma
CLICK HERE to watch Constantinos Hadjipanayis, MD, PhD, discuss his NIH-funded research.
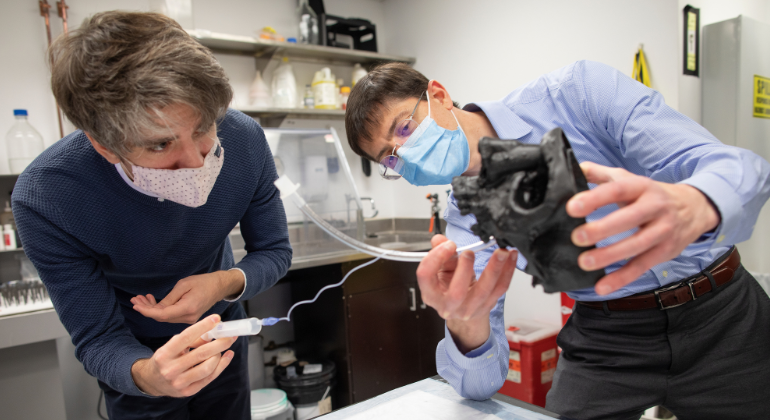
Dr. Hadjipanayis is the lead investigator in the $3.4 million National Institutes of Health (NIH)-funded study to examine the effects of MHT when used in conjunction with chemoradiation to treat glioblastoma, a devastating brain cancer that almost always relapses because therapy-resistant cancer cells infiltrate the body at the tumor’s margin. The study is expected to last five years and will be conducted in close partnership with Robert Ivkov, PhD, MSc, and his team at Johns Hopkins University, who developed the novel magnetic nanoparticles the studies will use. The grant involves a pilot study at Johns Hopkins treating dogs that have spontaneously developed glioblastoma tumors.
“These are powerful magnetic nanoparticles that we deliver directly into glioblastoma tumors by convection-enhanced delivery,” said Dr. Hadjipanayis. “We then apply a safe, alternating external magnetic field that oscillates the nanoparticles, which generates heat that destroys the tumor. Multiple treatments can be performed since the nanoparticles persist in glioblastoma tumors. When used in conjunction with radiation and chemotherapy, we expect this treatment will lead to improved outcomes.”
- Glioma Dormancy, Stem Cell Niche, and Tumor Microenvironment
Hongyan Zou, MD, PhD, Professor of Neurosurgery, and Neuroscience, at the Icahn School of Medicine at Mount Sinai, has received a $3 million NIH-funded grant to study tumor cell dormancy in glioblastoma models. The project’s goal is to dissect governing factors in the tumor microenvironment that influence tumor cell behaviors and therapy resistance. The study is expected to last five years.
“Tumor cell dormancy is a major root for glioblastoma relapse,” said Dr. Zou. “Our team of vascular biologists, bioengineers, and neuroscientists are employing a 3D vascular glioblastoma organoid model to understand governing factors in the tumor microenvironment that promote tumor stem cell dormancy, therapy resistance, and tumor re-propagating capacity.”
- Defining the Chromatin Landscape and Transcriptional Drivers of Proliferation and Migration in Human Glioblastoma
- Crosstalk between EGFR and TEAD Activity Directs Migration in Human Glioblastoma
A better understanding of the mechanisms by which glioblastoma cells infiltrate deep into the brain, evading surgical resection and chemotherapy, is needed in order to prevent tumor progression. Nadejda Tsankova, MD, PhD, Associate Professor of Pathology, and Neuroscience, at the Icahn School of Medicine at Mount Sinai, is the Principal Investigator on two studies that examine the biology of migration in glioblastoma cells. The first NIH-funded study aims to define the epigenetic landscape (nongenetic influences on gene expression) and transcriptional networks that drive properties of growth and migration in human glioblastoma cells. The second study focuses on the role of one specific transcription factor, the transcriptional enhanced associate domain (TEAD) as driver of the migratory tumor cell state, and explores its relationship to epidermal growth factor receptor (EGFR) signaling, using CRISPR-knockout and pharmacological inhibition in primary patient-derived glioblastoma cells and in immunocompetent and xenograft mouse glioma models. Dr. Tsankova has received nearly $275,000 for the first study and more than $1.8 million in funding for the second, five-year study.
“We have uncovered TEAD1 as an important driver of tumor migration,” said Dr. Tsankova. “Through our studies, we aim to gain deeper mechanistic insight into the biology of tumor migration as well as to test the therapeutic efficacy of pharmacological inhibitors of TEAD1 activity in pre-clinical mouse glioma models.”
- Molecular and cellular mechanisms of glioma invasion
Roland H. Friedel, PhD, Associate Professor of Neuroscience, and Neurosurgery, at the Icahn School of Medicine at Mount Sinai, is the Principal Investigator of an NIH-funded project ($1.8 million for a five-year period) to study signaling pathways that promote the migratory potential of glioblastoma invasion.
“Infiltrative growth of glioblastoma cells is a major determinant of high lethality of glioblastoma,” said Dr. Friedel. “We have been studying novel signaling pathways that drive tumor invasion. The ultimate goal is to develop novel therapies in combination with conventional chemo radiation to curb glioblastoma progression.”
About the Mount Sinai Health System
Mount Sinai Health System is one of the largest academic medical systems in the New York metro area, with 48,000 employees working across seven hospitals, more than 400 outpatient practices, more than 600 research and clinical labs, a school of nursing, and a leading school of medicine and graduate education. Mount Sinai advances health for all people, everywhere, by taking on the most complex health care challenges of our time—discovering and applying new scientific learning and knowledge; developing safer, more effective treatments; educating the next generation of medical leaders and innovators; and supporting local communities by delivering high-quality care to all who need it.
Through the integration of its hospitals, labs, and schools, Mount Sinai offers comprehensive health care solutions from birth through geriatrics, leveraging innovative approaches such as artificial intelligence and informatics while keeping patients’ medical and emotional needs at the center of all treatment. The Health System includes approximately 9,000 primary and specialty care physicians and 10 free-standing joint-venture centers throughout the five boroughs of New York City, Westchester, Long Island, and Florida. Hospitals within the System are consistently ranked by Newsweek’s® “The World’s Best Smart Hospitals, Best in State Hospitals, World Best Hospitals and Best Specialty Hospitals” and by U.S. News & World Report's® “Best Hospitals” and “Best Children’s Hospitals.” The Mount Sinai Hospital is on the U.S. News & World Report® “Best Hospitals” Honor Roll for 2025-2026.
For more information, visit https://www.mountsinai.org or find Mount Sinai on Facebook, Instagram, LinkedIn, X, and YouTube.
Artificial Intelligence Platform Screens for Acute Neurological Illnesses at Mount Sinai
Aug 13, 2018 View All Press Releases