Mount Sinai Scientists and International Team Shed New Light on Schizophrenia in Largest Genomic Study Published to Date
Genes and pathways identified could inform new approaches to treatment and address acute need for drug development for this disorder
As part of a multinational, collaborative effort, researchers from the Icahn School of Medicine at Mount Sinai have helped identify over 100 locations in the human genome associated with the risk of developing schizophrenia, in the largest genomic study published on any psychiatric disorder to date, conducted with 80,000 people. The findings, published online in Nature, point to biological mechanisms and pathways that may underlie schizophrenia, and could lead to new approaches to treating the disorder, which has seen little innovation in drug development in more than 60 years.
Schizophrenia, a debilitating psychiatric disorder that affects approximately 1 out of every 100 people worldwide, is characterized by hallucinations, paranoia, and a breakdown of thought processes, and often emerges in the teens and early 20s. Its lifetime impact on individuals and society is high, both in terms of years of healthy life lost to disability and in terms of financial cost, with studies estimating the cost of schizophrenia at over $60 billion annually in the U.S. alone.
“By studying the genome, we are getting a better handle on the genetic variations that are making people vulnerable to psychiatric disease," said Tom Insel, director of the National Institute of Mental Health, which helped fund the study. “Through the wonders of genomic technology, we are in a period in which, for the first time, we are beginning to understand many of the players at the molecular and cellular level.”
In the genome-wide association study (GWAS) published in Nature, the authors looked at over 80,000 genetic samples from schizophrenia patients and healthy volunteers and found 108 specific locations in the human genome associated with risk for schizophrenia. Eighty-three of those loci had not previously been linked to the disorder.
“Through its open and extensive worldwide data sharing policies, The Psychiatric Genomics Consortium (PGC), which led this work, is having a major impact on our understanding of schizophrenia. Without these efforts it would have been impossible to gather and analyze DNA data from enough people with and without schizophrenia,” said Pamela Sklar, MD, PhD, co-author of the study, Chief of the Division of Psychiatric Genomics and Professor of Psychiatry at the Icahn School of Medicine at Mount Sinai.
The study implicates genes expressed in brain tissue, particularly those related to neuronal and synaptic function. These include genes that are active in pathways controlling synaptic plasticity – a function essential to learning and memory – and pathways governing postsynaptic activity, such as voltage-gated calcium channels, which are involved in signaling between cells in the brain. These newly identified loci may point to additional therapeutic targets.
“The fact that we were able to detect genetic risk factors on this massive scale shows that schizophrenia can be tackled by the same approaches that have already transformed our understanding of other diseases,” said paper co-author Michael O’Donovan, deputy director of the MRC Centre for Neuropsychiatric Genetics and Genomics at Cardiff University School of Medicine. ‘The wealth of new findings have the potential to kick-start the development of new treatments in schizophrenia, a process which has stalled for the last 60 years.”
The study is the result of several years of work by the Schizophrenia Working Group of the Psychiatric Genomics Consortium (PGC, http://pgc.unc.edu), an international, multi-institutional collaboration founded in 2007 to conduct broad-scale analyses of genetic data for psychiatric disease. The current paper used 55 datasets from more than 40 different contributors to conduct the analysis. The DNA data from the 80,000 people used in this study represent all the data that the consortium has amassed to date. The PGC is currently genotyping over 100,000 additional people to further study schizophrenia and other psychiatric diseases, including autism and bipolar disorder.
Core funding for the Psychiatric Genomics Consortium comes from the U.S. National Institute of Mental Health (NIMH), along with numerous grants from governmental and charitable organizations, as well as philanthropic donations.
Paper cited:
Schizophrenia Working Group of the Psychiatric Genomics Consortium. “Biological insights from 108 schizophrenia-associated genetic loci.” Nature. DOI: 10.1038/nature13595. In Press.
About the Mount Sinai Health System
Mount Sinai Health System is one of the largest academic medical systems in the New York metro area, with 48,000 employees working across seven hospitals, more than 400 outpatient practices, more than 600 research and clinical labs, a school of nursing, and a leading school of medicine and graduate education. Mount Sinai advances health for all people, everywhere, by taking on the most complex health care challenges of our time—discovering and applying new scientific learning and knowledge; developing safer, more effective treatments; educating the next generation of medical leaders and innovators; and supporting local communities by delivering high-quality care to all who need it.
Through the integration of its hospitals, labs, and schools, Mount Sinai offers comprehensive health care solutions from birth through geriatrics, leveraging innovative approaches such as artificial intelligence and informatics while keeping patients’ medical and emotional needs at the center of all treatment. The Health System includes approximately 9,000 primary and specialty care physicians and 10 free-standing joint-venture centers throughout the five boroughs of New York City, Westchester, Long Island, and Florida. Hospitals within the System are consistently ranked by Newsweek’s® “The World’s Best Smart Hospitals, Best in State Hospitals, World Best Hospitals and Best Specialty Hospitals” and by U.S. News & World Report's® “Best Hospitals” and “Best Children’s Hospitals.” The Mount Sinai Hospital is on the U.S. News & World Report® “Best Hospitals” Honor Roll for 2025-2026.
For more information, visit https://www.mountsinai.org or find Mount Sinai on Facebook, Instagram, LinkedIn, X, and YouTube.
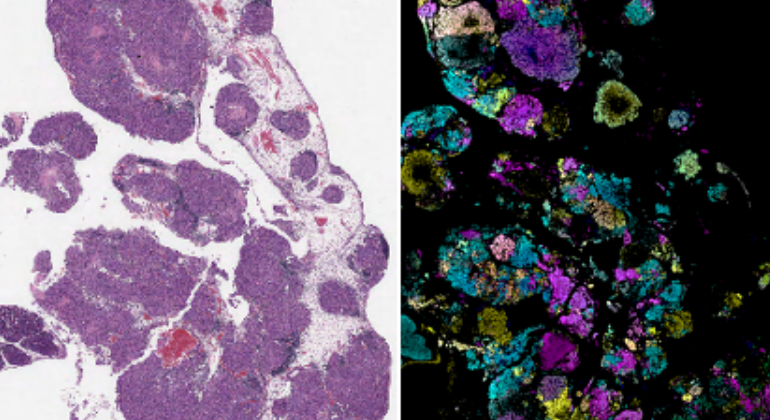
Mount Sinai Researchers Uncover Why Some Leukemia Cells May Resist Treatment
Oct 30, 2024 View All Press Releases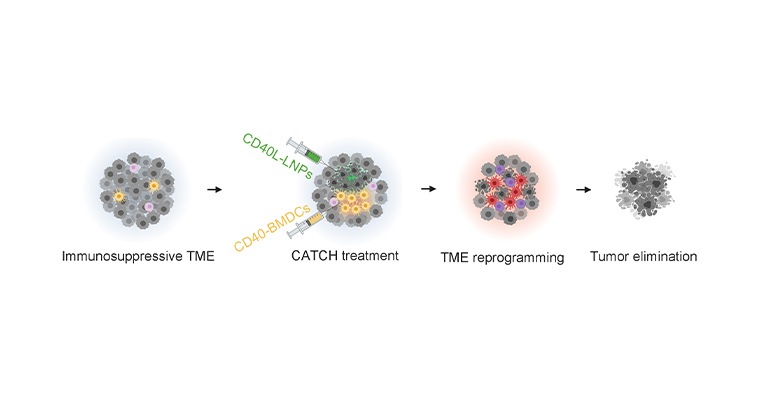
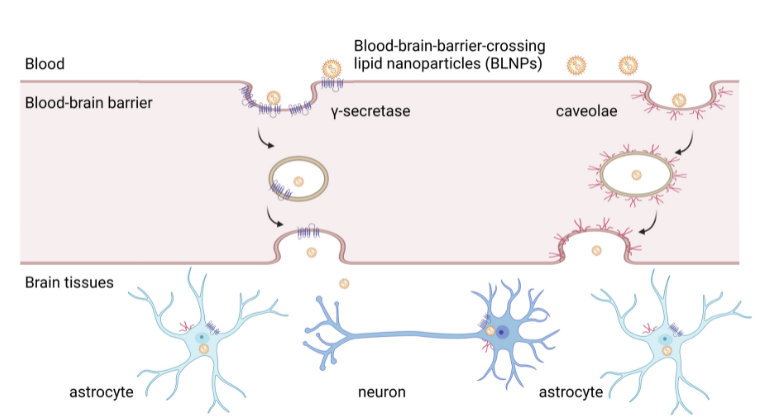
New RNA-based Therapy Combats Melanoma in Mouse Models
Jul 27, 2023 View All Press Releases
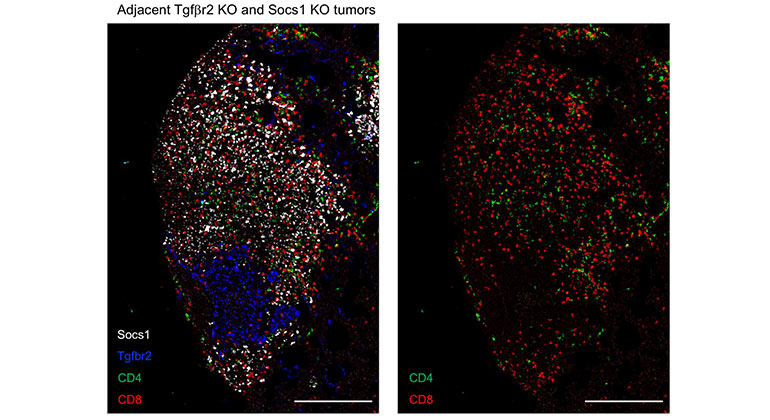
Targeting One Type of Immune Cell With Another Slows Cancer Growth in Preclinical Studies
Oct 25, 2022 View All Press Releases
Novel CRISPR Imaging Technology Reveals Genes Controlling Tumor Immunity
Mar 15, 2022 View All Press Releases