Mount Sinai Scientists Uncover Link Between Influenza and Heart Disease
New study results could lead to mRNA therapeutic to reduce the risk of cardiac damage
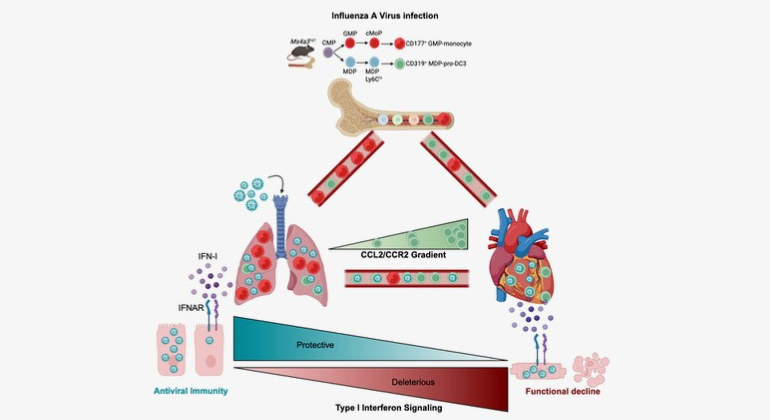
Graphical Abstract summarizing the key findings of the paper. The authors found that severe influenza damages the heart by exploiting a specific immune cells and engaging a type-I interferon response. The authors also show that therapeutic silencing of the response mitigates heart damage.
Mount Sinai researchers have identified a cellular mechanism linking infections from influenza A viruses (IAVs) to cardiovascular disease, providing critical insights on how influenza can damage the heart and increase the risk of a heart attack or other major cardiovascular event.
Through its work with mouse models and human data, the team also provided evidence that a cutting-edge modified mRNA treatment that dampens an interferon signaling pathway in the heart can significantly mitigate cardiac damage following viral infection while preserving the protective antiviral response of the immune system. The study was published in the February 9 issue of Immunity.
“We have known for years that the frequency of heart attacks increases during flu season, yet outside of clinical intuition, scant evidence exists of the underlying mechanisms of that phenomenon,” says Filip Swirski, PhD, Director of the Cardiovascular Research Institute at the Icahn School of Medicine at Mount Sinai and the senior author of the study. “Studies like ours are now shedding valuable light on immune system pathways, like the antiviral cytokine type 1 interferon (IFN-1), that factor into damage to the heart following severe influenza infection. These findings offer great promise for the development of new therapies, which are desperately needed since there are currently no viable clinical options to prevent cardiac damage.”
Influenza A viruses are responsible for an estimated 1 billion infections globally each year, ranging from seasonal flu outbreaks locally to pandemics globally. While most infections are mild and self-resolving, in some cases they can become severe or even fatal, particularly when the virus travels to the heart and triggers the death of cardiomyocytes, specialized muscle cells that are responsible for the rhythmic contraction and relaxation of the heart.
The Mount Sinai team studied autopsies of 35 hospitalized patients who died of influenza and found that more than 85 percent had at least one significant cardiovascular comorbidity, such as hypertension, and that the majority had multiple comorbidities, including atherosclerosis and cardiac fibrosis, underscoring cardiovascular disease as a major driver of influenza mortality.
The research team also uncovered the mechanism by which cardiac damage occurs. They learned, for example, that a novel subset of white blood cells, known as pro-dendritic cell 3, becomes infected in the lung and, after traveling to the heart, produces large amounts of type 1 interferon. This, instead of fulfilling its mission of clearing the virus from the heart, triggers the death of cardiomyocytes, impairing cardiac output.
“We found that the pro-dendritic cell 3 acts as the ‘Trojan horse’ of the immune system during influenza infection, becoming infected in the lung, trafficking the virus to the heart, and disseminating it to cardiomyocytes. This process causes production of the damaging type 1 interferon that comes with considerable collateral damage to the heart,” explains Jeffrey Downey, PhD, a member of Dr. Swirski’s laboratory who served as lead author of the study. “The hopeful news for patients is that by injecting a novel mod-RNA therapeutic that modulates the IFN-1 signaling pathway, we reduced levels of cardiac damage, as evidenced by lower troponin, and improved cardiac function, as measured by higher left ventricular ejection fraction.”
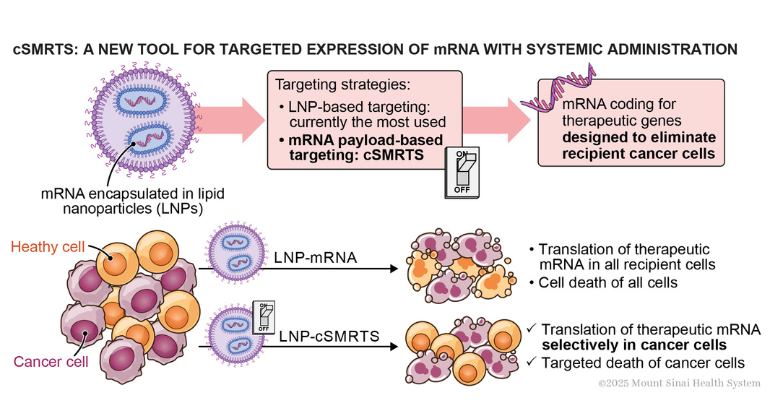
As part of its ongoing research, Dr. Swirski’s team is collaborating with Lior Zangi, PhD, Associate Professor of Medicine (Cardiology), and Genetics and Genomic Sciences, at the Icahn school of Medicine at Mount Sinai, to investigate the use of a safe and effective systemic delivery method of the mod-RNA therapeutic to the heart’s muscle cells, instead of the direct injection method used in its proof-of-concept study. Additional work is focused on the pro-dendritic cell 3 itself: why is it so susceptible to influenza and how could its protective capacity be fully harnessed to potentially minimize heart damage exacerbated by cardiovascular disease?
“Pathogens are constantly emerging and evolving, which means our strategies to combat them must evolve as well,” says Dr. Swirski. “Better understanding of influenza pathogenesis and immune pathways that are activated throughout the body will help fuel the next stage of advanced care.”
This study was principally supported by the following grants from the National Heart, Lung, and Blood Institute and the Charles H. Revson Foundation: P01HL131478, P01 HL142494, R01 HL178835, K99 HL177314, and 24-29.
Mount Sinai Is a World Leader in Cardiology and Heart Surgery
Mount Sinai Fuster Heart Hospital at The Mount Sinai Hospital ranks No. 2 nationally for cardiology, heart, and vascular surgery, according to U.S. News & World Report®. It also ranks No. 1 in New York and No. 6 globally according to Newsweek’s “The World’s Best Specialized Hospitals.”
It is part of Mount Sinai Health System, which is New York City's largest academic medical system, encompassing seven hospitals, a leading medical school, and a vast network of ambulatory practices throughout the greater New York region. We advance medicine and health through unrivaled education and translational research and discovery to deliver care that is the safest, highest-quality, most accessible and equitable, and the best value of any health system in the nation. The Health System includes approximately 9,000 primary and specialty care physicians; 10 free-standing joint-venture centers throughout the five boroughs of New York City, Westchester, Long Island, and Florida; and 48 multidisciplinary research, educational, and clinical institutes. Hospitals within the Health System are consistently ranked by Newsweek’s® “The World’s Best Smart Hospitals” and by U.S. News & World Report's® “Best Hospitals” and “Best Children’s Hospitals.” The Mount Sinai Hospital is on the U.S. News & World Report's® “Best Hospitals” Honor Roll for 2025-2026.
For more information, visit https://www.mountsinai.org or find Mount Sinai on Facebook, Instagram, LinkedIn, X, and YouTube.
About the Mount Sinai Health System
Mount Sinai Health System is one of the largest academic medical systems in the New York metro area, with 48,000 employees working across seven hospitals, more than 400 outpatient practices, more than 600 research and clinical labs, a school of nursing, and a leading school of medicine and graduate education. Mount Sinai advances health for all people, everywhere, by taking on the most complex health care challenges of our time—discovering and applying new scientific learning and knowledge; developing safer, more effective treatments; educating the next generation of medical leaders and innovators; and supporting local communities by delivering high-quality care to all who need it.
Through the integration of its hospitals, labs, and schools, Mount Sinai offers comprehensive health care solutions from birth through geriatrics, leveraging innovative approaches such as artificial intelligence and informatics while keeping patients’ medical and emotional needs at the center of all treatment. The Health System includes approximately 9,000 primary and specialty care physicians and 10 free-standing joint-venture centers throughout the five boroughs of New York City, Westchester, Long Island, and Florida. Hospitals within the System are consistently ranked by Newsweek’s® “The World’s Best Smart Hospitals, Best in State Hospitals, World Best Hospitals and Best Specialty Hospitals” and by U.S. News & World Report's® “Best Hospitals” and “Best Children’s Hospitals.” The Mount Sinai Hospital is on the U.S. News & World Report® “Best Hospitals” Honor Roll for 2025-2026.
For more information, visit https://www.mountsinai.org or find Mount Sinai on Facebook, Instagram, LinkedIn, X, and YouTube.
Scientists Develop a Smarter mRNA Therapy That Knows Which Cells to Target
Dec 15, 2025 View All Press Releases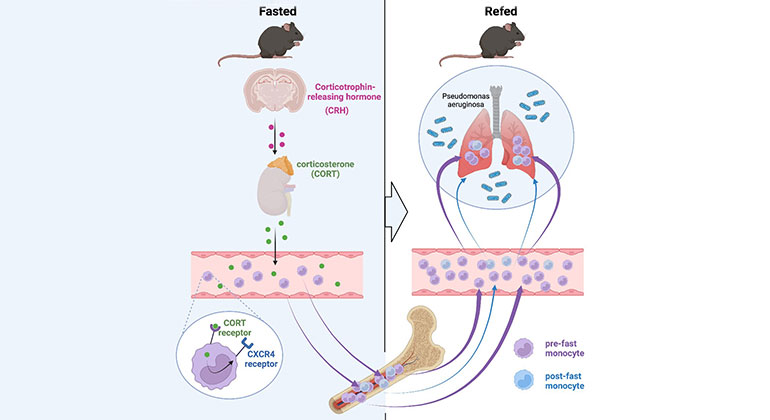
Skipping Breakfast May Compromise the Immune System
Feb 23, 2023 View All Press Releases
Mount Sinai Recruits Internationally Recognized Cardiovascular Immunology Researcher
Jul 21, 2021 View All Press Releases.jpg)