New Insights About Brain Receptor May Pave Way for Next-Gen Mental Health Drugs
Study sheds light on elusive 5-HT1A serotonin receptor, a target of antidepressants and psychedelics
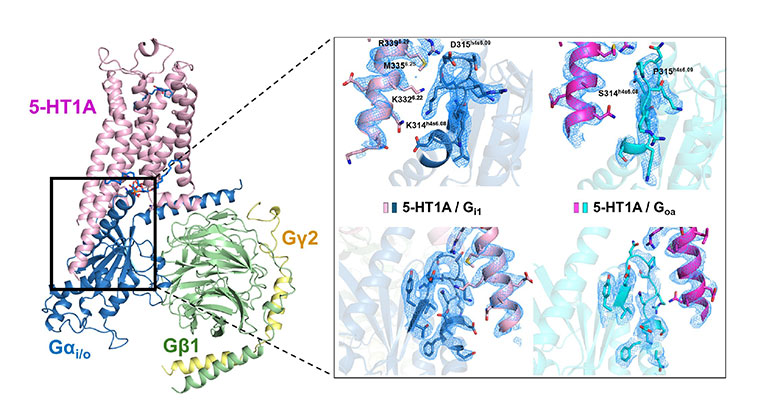
High-resolution 3D image showing how the 5-HT1A receptor connects with internal signaling proteins (G proteins). The highlighted areas reveal key contact points between the receptor and two different types of G proteins, captured using advanced cryo-electron microscopy. From A.L Warren et al., Structural determinants of G protein subtype selectivity at the serotonin receptor 5-HT1A. Science Advances. 2025. This work is licensed under CC BY-NC 4.0 (https://creativecommons.org/licenses/by-nc/4.0/).
In a discovery that could guide the development of next-generation antidepressants and antipsychotic medications, researchers at the Icahn School of Medicine at Mount Sinai have developed new insights into how a critical brain receptor works at the molecular level and why that matters for mental health treatments.
The study, published in the August 1 online issue of Science Advances [10.1126/sciadv.adu9851], focuses on the 5-HT1A serotonin receptor, a major player in regulating mood and a common target of both traditional antidepressants and newer therapies such as psychedelics. Despite its clinical importance, this receptor has remained poorly understood, with many of its molecular and pharmacological properties largely understudied—until now.
“This receptor is like a control panel that helps manage how brain cells respond to serotonin, a key chemical involved in mood, emotion, and cognition,” says senior author Daniel Wacker, PhD, Assistant Professor of Pharmacological Sciences, and Neuroscience, at the Icahn School of Medicine at Mount Sinai. “Our findings shed light on how that control panel operates—what switches it flips, how it fine-tunes signals, and where its limits lie. This deeper understanding could help us design better therapies for mental health conditions like depression, anxiety, and schizophrenia.”
Using innovative lab techniques, the research team discovered that the 5-HT1A receptor is inherently wired to favor certain cellular signaling pathways over others—regardless of the drug used to target it. However, drugs can still influence the strength with which those pathways are activated. For example, the antipsychotic asenapine (brand name Saphris) was found to selectively engage a specific signaling route due to its relatively weak activity at the receptor.
To explore these mechanisms in greater detail, the researchers combined experiments in lab-grown cells with high-resolution cryo-electron microscopy—a cutting-edge imaging technology that reveals molecular structures at near-atomic resolution. Their work focused on how various drugs activate the 5-HT1A receptor and how the receptor interacts with internal signaling proteins known as G proteins.
Different signaling pathways controlled by the 5-HT1A receptor are linked to different aspects of mood, perception, and even pain. As scientists better understand which pathways are activated, and how, they can more precisely design drugs that treat specific symptoms or conditions without unwanted side effects.
“Our work provides a molecular map of how different drugs ‘push buttons’ on this receptor—activating or silencing specific pathways that influence brain function,” says study first author Audrey L. Warren, PhD, a former student in Dr. Wacker’s lab who is now a postdoctoral researcher at Columbia University. “By understanding exactly how these drugs interact with the receptor, we can start to predict which approaches might lead to more effective or targeted treatments and which ones are unlikely to work. It’s a step toward designing next-generation therapies with greater precision and fewer side effects.”
In a particularly surprising finding, the researchers discovered that a phospholipid—a type of fat molecule found in cell membranes—plays a major role in steering the receptor’s activity, almost like a hidden co-pilot. This is the first time such a role has been observed among the more than 700 known receptors of this type in the human body.
While current antidepressants often take weeks to work, scientists hope this new understanding of 5-HT1A signaling could help explain those delays and lead to faster-acting alternatives.
“This receptor may help explain why standard antidepressants take long to work,” says Dr. Wacker. “By understanding how it functions at a molecular level, we have a clearer path to designing faster, more effective treatments, not just for depression, but also for conditions like psychosis and chronic pain. It’s a key piece of the puzzle.”
Next, the research team plans to dig deeper into the role of the phospholipid "co-factor" and to test how their lab-based findings hold up in more complex experiments. They're also working on turning these discoveries into real-world compounds that could become future psychiatric medications, building on their earlier success with drug candidates derived from psychedelics.
The paper is titled “Structural determinants of G protein subtype selectivity at the serotonin receptor 5-HT1A.”
The study’s authors, as listed in the journal, are Audrey L. Warren, Gregory Zilberg, Anwar Abbassi, Alejandro Abraham, Shifan Yang, and Daniel Wacker.
This work was supported by NIH grant GM133504. Further support came from NIH T32 Training Grant GM062754 and DA053558 and NIH F31 fellowship MH132317.
About the Mount Sinai Health System
Mount Sinai Health System is one of the largest academic medical systems in the New York metro area, with 48,000 employees working across seven hospitals, more than 400 outpatient practices, more than 600 research and clinical labs, a school of nursing, and a leading school of medicine and graduate education. Mount Sinai advances health for all people, everywhere, by taking on the most complex health care challenges of our time—discovering and applying new scientific learning and knowledge; developing safer, more effective treatments; educating the next generation of medical leaders and innovators; and supporting local communities by delivering high-quality care to all who need it.
Through the integration of its hospitals, labs, and schools, Mount Sinai offers comprehensive health care solutions from birth through geriatrics, leveraging innovative approaches such as artificial intelligence and informatics while keeping patients’ medical and emotional needs at the center of all treatment. The Health System includes approximately 9,000 primary and specialty care physicians and 10 free-standing joint-venture centers throughout the five boroughs of New York City, Westchester, Long Island, and Florida. Hospitals within the System are consistently ranked by Newsweek’s® “The World’s Best Smart Hospitals, Best in State Hospitals, World Best Hospitals and Best Specialty Hospitals” and by U.S. News & World Report's® “Best Hospitals” and “Best Children’s Hospitals.” The Mount Sinai Hospital is on the U.S. News & World Report® “Best Hospitals” Honor Roll for 2025-2026.
For more information, visit https://www.mountsinai.org or find Mount Sinai on Facebook, Instagram, LinkedIn, X, and YouTube.