Mount Sinai Researchers Identify and Characterize Three Molecular Subtypes of Alzheimer’s Disease
Critical Step Toward Developing Precision Medicine Treatments
Researchers at the Icahn School of Medicine at Mount Sinai have identified three major molecular subtypes of Alzheimer’s disease (AD) using data from RNA sequencing. The study advances our understanding of the mechanisms of AD and could pave the way for developing novel, personalized therapeutics.
The work was funded by the National Institute on Aging, part of the National Institutes of Health (NIH), and published in Science Advances on January 6, 2021.
RNA is a genetic molecule similar to DNA that encodes the instructions for making proteins. RNA sequencing is a technology that reveals the presence and quantity of RNA in a biological sample such as a brain slice.
Alzheimer’s disease is the most common form of dementia, but it is quite diverse in its biological and pathological manifestations. There is growing evidence that disease progression and responses to interventions differ significantly among Alzheimer’s patients. Some patients have slow cognitive decline while others decline rapidly; some have significant memory loss and an inability to remember new information while others do not; and some patients experience psychosis and/or depression associated with AD while others do not.
“Such differences strongly suggest there are subtypes of AD with different biological and molecular factors driving disease progression,” said Bin Zhang, PhD, the lead author of the study, Director of the Center for Transformative Disease Modeling, and Professor of Genetics and Genomic Sciences at the Icahn School of Medicine.
To identify the molecular subtypes of AD, the researchers used a computational biology approach to illuminate the relationships among different types of RNA, clinical and pathological traits, and other biological factors that potentially drive the disease’s progress. The research team analyzed RNA-sequencing data of more than 1,500 samples across five brain regions from hundreds of deceased patients with AD and normal controls, and identified three major molecular subtypes of AD. These AD subtypes were independent of age and disease stage, and were replicated across multiple brain regions in two cohort studies.
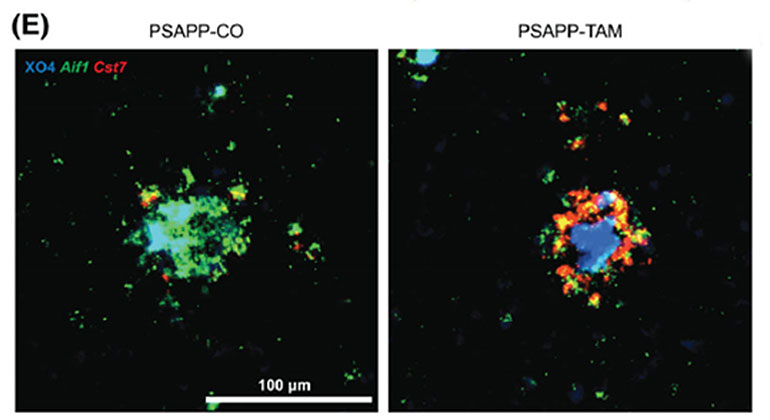
These subtypes correspond to different combinations of multiple dysregulated biological pathways leading to brain degeneration. Tau neurofibrillary tangle and amyloid-beta plaque, two neuropathological hallmarks of AD, are significantly increased only in certain subtypes.
Many recent studies have shown that an elevated immune response may help cause Alzheimer’s. However, more than half of AD brains don’t show increased immune response compared to normal healthy brains. The analysis further revealed subtype-specific molecular drivers in AD progression in these samples. The research also identified the correspondence between these molecular subtypes and the existing AD animal models used for mechanistic studies and for testing candidate therapeutics, which may partially explain why a vast majority of drugs that succeeded in certain mouse models failed in human AD trials, which likely had participants belonging to different molecular subtypes.
Although the subtyping described by the researchers was performed post mortem using the patients’ brain tissue, the researchers said that if the findings were validated by future studies, they could lead to the identification in living patients of biomarkers and clinical features associated with these molecular subtypes and earlier diagnosis and intervention.
“Our systematic identification and characterization of the robust molecular subtypes of AD reveal many new signaling pathways dysregulated in AD and pinpoint new targets,” said Dr. Zhang, “These findings lay down a foundation for determining more effective biomarkers for early prediction of AD, studying causal mechanisms of AD, developing next-generation therapeutics for AD and designing more effective and targeted clinical trials, ultimately leading to precision medicine for AD. The remaining challenges for future research include replication of the findings in larger cohorts, validation of subtype specific targets and mechanisms, identification of peripheral biomarkers and clinical features associated with these molecular subtypes.”
The AD subtyping study is supported by the NIH National Institute on Aging (NIA) and is part of the NIA-led Accelerating Medicines Partnership - Alzheimer's Disease (AMP-AD) Target Discovery and Preclinical Validation program. This public private partnership aims to shorten the time between the discovery of potential drug targets and the development of new drugs for Alzheimer’s disease treatment and prevention.
About the Mount Sinai Health System
Mount Sinai Health System is one of the largest academic medical systems in the New York metro area, with 48,000 employees working across seven hospitals, more than 400 outpatient practices, more than 600 research and clinical labs, a school of nursing, and a leading school of medicine and graduate education. Mount Sinai advances health for all people, everywhere, by taking on the most complex health care challenges of our time—discovering and applying new scientific learning and knowledge; developing safer, more effective treatments; educating the next generation of medical leaders and innovators; and supporting local communities by delivering high-quality care to all who need it.
Through the integration of its hospitals, labs, and schools, Mount Sinai offers comprehensive health care solutions from birth through geriatrics, leveraging innovative approaches such as artificial intelligence and informatics while keeping patients’ medical and emotional needs at the center of all treatment. The Health System includes approximately 9,000 primary and specialty care physicians and 10 free-standing joint-venture centers throughout the five boroughs of New York City, Westchester, Long Island, and Florida. Hospitals within the System are consistently ranked by Newsweek’s® “The World’s Best Smart Hospitals, Best in State Hospitals, World Best Hospitals and Best Specialty Hospitals” and by U.S. News & World Report's® “Best Hospitals” and “Best Children’s Hospitals.” The Mount Sinai Hospital is on the U.S. News & World Report® “Best Hospitals” Honor Roll for 2025-2026.
For more information, visit https://www.mountsinai.org or find Mount Sinai on Facebook, Instagram, LinkedIn, X, and YouTube.
Researchers Identify the Role of an Alzheimer’s Disease Risk Gene in the Brain
Nov 30, 2022 View All Press Releases
Scientists Show How Bone-Bordering Cells May Help Shape a Skull
Dec 09, 2021 View All Press ReleasesMount Sinai Researchers Uncover New Molecular Drivers of Parkinson’s Disease
Nov 20, 2019 View All Press Releases