Liver Cancer Tumors Appear to Be Resistant to Immunotherapy in Patients With Underlying Non-alcoholic Steatohepatitis (NASH)
Immunotherapy also appears to fuel tumor growth in these cancers
Immunotherapy is not only significantly less effective in liver cancer patients who previously had a liver disease called non-alcoholic steatohepatitis (NASH), but actually appears to fuel tumor growth, according to a Mount Sinai study published in Nature in March. NASH affects as many as 40 million people worldwide and is associated with obesity and diabetes.
The researchers led a large international collaboration to investigate immunotherapy’s effect on hepatocellular carcinoma (HCC), a deadly liver cancer, caused by NASH. They conducted a meta-analysis of three randomized phase 3 human trials that tested immunotherapy in HCC and found that in non-viral HCC cases, such as NASH-related HCC, therapy was significantly less effective than in viral-related cases.
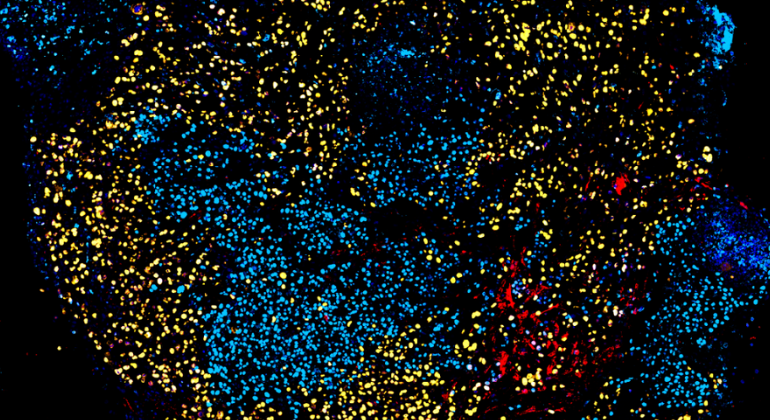
In addition, this study found in animal models that immunotherapy with anti-PD1 inhibitors actually led to tumor growth instead of the intended effect of aiding the immune system to kill cancer cells and shrink the tumor. In these models, researchers identified immune cells called CD8+PD1+ as drivers of these phenomena. These cells were found to be dysfunctional and incapable of immunosurveillance.
“In addition to allowing clinicians to optimize treatment protocols based on the underlying liver disease, the knowledge obtained through this study will provide a backbone for the design of further combination treatments to overcome current limitations and improve survival for patients with these underlying liver conditions,” said senior and co-corresponding author Josep Llovet, MD, PhD, Founder and Director of the Liver Cancer Program at The Tisch Cancer Institute and Professor of Medicine (Liver Diseases) at the Icahn School of Medicine at Mount Sinai. “These results also highlight the need for refined therapeutic strategies aimed at treating both the tumor as well as the microenvironment associated with distinct underlying liver disease.”
Non-alcoholic fatty liver disease (NAFLD), a condition that is a precursor of NASH, is estimated to affect 25 percent of the population worldwide, and up to 20 percent of these patients will progress to having NASH. NASH is an emerging risk factor for HCC, which led to this study’s investigation of immunotherapy’s effects on NASH-related HCC. While immunotherapy has clinical benefit for hepatocellular carcinoma, this study’s findings are important because a quarter of all HCC patients have NASH.
The meta-analysis in this study was conducted on three high-quality phase 3 trials that included more than 1,600 HCC patients treated with anti-PD1 immunotherapy. This study represents a major international collaborative effort from 110 investigators from 81 institutions.
Amaia Lujambio, PhD; Thomas Marron, MD, PhD; and Philipp Haber, MD, from Mount Sinai contributed significantly to this study and are also co-authors.
About the Mount Sinai Health System
Mount Sinai Health System is one of the largest academic medical systems in the New York metro area, with 48,000 employees working across seven hospitals, more than 400 outpatient practices, more than 600 research and clinical labs, a school of nursing, and a leading school of medicine and graduate education. Mount Sinai advances health for all people, everywhere, by taking on the most complex health care challenges of our time—discovering and applying new scientific learning and knowledge; developing safer, more effective treatments; educating the next generation of medical leaders and innovators; and supporting local communities by delivering high-quality care to all who need it.
Through the integration of its hospitals, labs, and schools, Mount Sinai offers comprehensive health care solutions from birth through geriatrics, leveraging innovative approaches such as artificial intelligence and informatics while keeping patients’ medical and emotional needs at the center of all treatment. The Health System includes approximately 9,000 primary and specialty care physicians and 10 free-standing joint-venture centers throughout the five boroughs of New York City, Westchester, Long Island, and Florida. Hospitals within the System are consistently ranked by Newsweek’s® “The World’s Best Smart Hospitals, Best in State Hospitals, World Best Hospitals and Best Specialty Hospitals” and by U.S. News & World Report's® “Best Hospitals” and “Best Children’s Hospitals.” The Mount Sinai Hospital is on the U.S. News & World Report® “Best Hospitals” Honor Roll for 2025-2026.
For more information, visit https://www.mountsinai.org or find Mount Sinai on Facebook, Instagram, LinkedIn, X, and YouTube.
Breakthrough Treatment for Liver Cancer Shows Big Promise in Global Study
Jan 09, 2025 View All Press Releases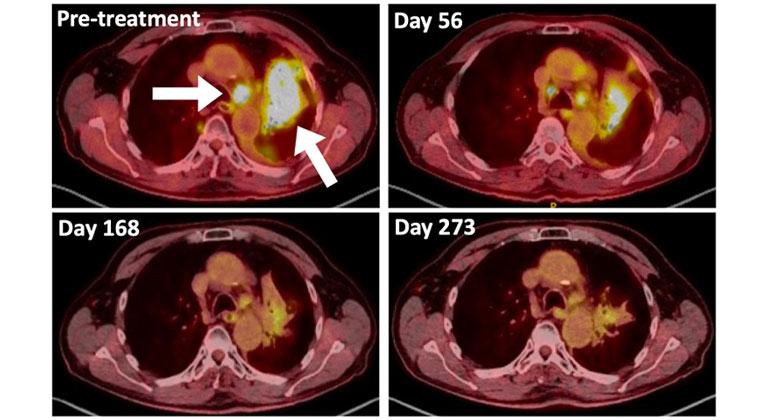
A Type of Allergy Medicine Might Help Treat Lung Cancer, Research Suggests
Dec 06, 2023 View All Press Releases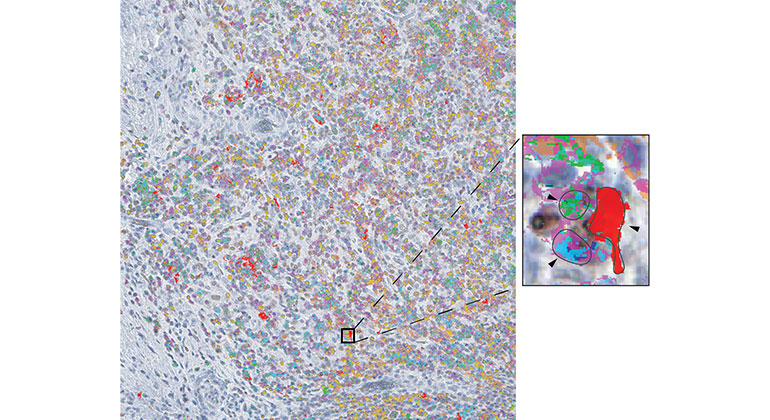
Study Reveals a Trio of Immune Cells Vital in Response to Liver Cancer Immunotherapy
Jun 15, 2023 View All Press ReleasesLibtayo effective in killing HCC tumors prior to resection
Jan 19, 2022 View All Press Releases