LVAD Patients Benefit from Heart Injection with Millions of Powerful Cells
New Study results presented at AHA Scientific Sessions 2013 show a single dose of stem cell therapy during surgery may improve new LVAD patients' heart function.
A multicenter team of researchers within the NIH-funded Cardiothoracic Surgical Trials Network (CTSN), led by Icahn School of Medicine at Mount Sinai, have found end-stage heart failure patients who receive a surgically implanted left ventricular assist device (LVAD) heart pump may also benefit from a single dose of millions of powerful cells injected directly into their heart during surgery.
The CTSN, whose Data and Clinical Coordinating Center is at Icahn School of Medicine at Mount Sinai, conducted the clinical trial in collaboration with the Cardiovascular Cell Therapy Research Network.
Allogeneic mesenchymal precursor cells (MPCs), are a subpopulation of adult mesenchymal stem cells, which when harvested from a healthy donor's bone marrow can be selected and expanded in the laboratory into hundreds of millions of MPCs.
At the American Heart Association Scientific Sessions 2013 on November 18, Icahn School of Medicine at Mount Sinai's research team presented the new findings for this novel, first-ever randomized, double-blinded multicenter trial assessing the safety and efficacy of injecting a single dose of 25 million MPCs directly into the heart muscle of advanced heart failure patients receiving an LVAD for either bridge-to-transplant or as a destination therapy.
Study results show one dose of the MPC therapy may contribute to improved heart muscle recovery in advanced heart failure patients who received an LVAD. In their study, researchers reported that 50 percent of patients who received MPCs were able to tolerate temporarily turning down their LVAD heart pump, compared to 20 percent of the placebo patients. In addition, no patients developed serious side effects that may be associated with the stem cell injections.
"These clinical trial results provide important data about the safety and potential efficacy of a single MPC injection at the time of LVAD implantation,” says the study's lead author Deborah D. Ascheim, MD, Associate Professor of Health Evidence and Policy and Cardiology at Icahn School of Medicine at Mount Sinai, who serves as Co-Director of the Data and Clinical Coordinating Center based at Mount Sinai for the NIH-sponsored Cardiothoracic Surgical Trials Network (CTSN) who conducted the clinical trial study.
"These mesenchymal precursor cells have shown their potential to safely facilitate early heart tissue repair in advanced heart failure. We look forward to investigating the benefits of this cell therapy further,” says Dr. Ascheim.
The thirty LVAD patients enrolled in the clinical trial were randomized 2:1 at 11 clinical sites to evaluate the single dose injection of MPCs. Patients were assigned to either receive an injection of 25 million MPCs, or a placebo. All patients were followed until a heart transplant was received or until one-year.
The CTSN has eight core clinical centers across the country. It's Data and Clinical Coordinating Center, based at Icahn School of Medicine at Mount Sinai, leads each of its clinical trial's design, methodologies, ethical research concerns, study data, analysis, and data reporting.
The company that makes this experimental MPC therapy is Mesoblast, Inc.
This study was presented at the AHA Scientific Sessions as a Clinical Science Special Report (Abstract 19673): Intramyocardial Injection of Allogeneic Mesenchymal Precursor Cells in Left Ventricular Assist Device Patients.
About the Mount Sinai Health System
Mount Sinai Health System is one of the largest academic medical systems in the New York metro area, with 48,000 employees working across seven hospitals, more than 400 outpatient practices, more than 600 research and clinical labs, a school of nursing, and a leading school of medicine and graduate education. Mount Sinai advances health for all people, everywhere, by taking on the most complex health care challenges of our time—discovering and applying new scientific learning and knowledge; developing safer, more effective treatments; educating the next generation of medical leaders and innovators; and supporting local communities by delivering high-quality care to all who need it.
Through the integration of its hospitals, labs, and schools, Mount Sinai offers comprehensive health care solutions from birth through geriatrics, leveraging innovative approaches such as artificial intelligence and informatics while keeping patients’ medical and emotional needs at the center of all treatment. The Health System includes approximately 9,000 primary and specialty care physicians and 10 free-standing joint-venture centers throughout the five boroughs of New York City, Westchester, Long Island, and Florida. Hospitals within the System are consistently ranked by Newsweek’s® “The World’s Best Smart Hospitals, Best in State Hospitals, World Best Hospitals and Best Specialty Hospitals” and by U.S. News & World Report's® “Best Hospitals” and “Best Children’s Hospitals.” The Mount Sinai Hospital is on the U.S. News & World Report® “Best Hospitals” Honor Roll for 2025-2026.
For more information, visit https://www.mountsinai.org or find Mount Sinai on Facebook, Instagram, LinkedIn, X, and YouTube.
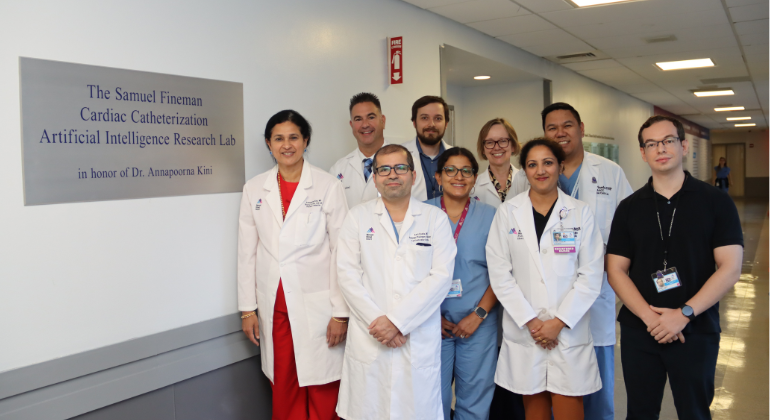
Mount Sinai Launches Cardiac Catheterization Artificial Intelligence Research Lab
Sep 15, 2025 View All Press Releases
Mount Sinai Surgeons Perform First Heart-Liver-Kidney Transplants in New York State
May 20, 2025 View All Press Releases