AI Model Improves Delirium Prediction, Leading to Better Health Outcomes for Hospitalized Patients
Novel AI Model boosts early detection and treatment by increasing staff efficiency
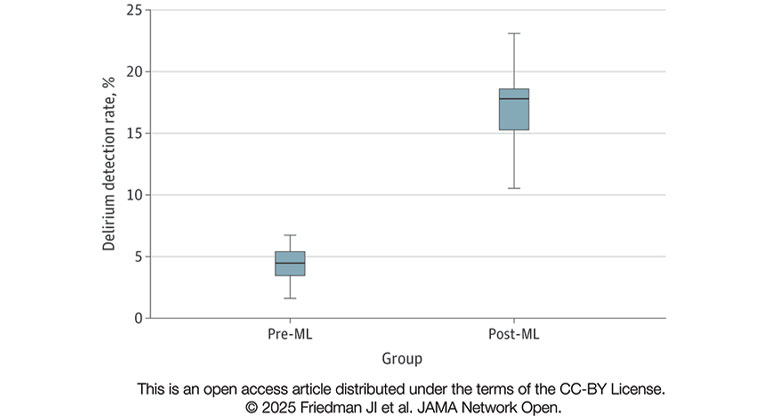
Comparison of monthly delirium detection rates before any ML-model deployment (pre-ML) and following deployment of the multimodal ML-delirium risk stratification model in live clinical practice (post-ML).
An artificial intelligence (AI) model improved outcomes in hospitalized patients by quadrupling the rate of detection and treatment of delirium. The model identifies patients at high risk for delirium and alerts a specially-trained team to assess the patient and create a treatment plan, if needed.
The model, developed by researchers at the Icahn School of Medicine at Mount Sinai, has been integrated into hospital operations, helping health care providers identify and manage delirium, a condition that can affect up to one-third of hospitalized patients.
The study, the first to show that an AI-powered delirium risk assignment model can not only perform well in a laboratory setting but also deliver real-world benefits in clinical practice, was published in the May 7, 2025 online issue of JAMA Network Open.
Delirium is a sudden and severe state of confusion that carries life-threatening risks and often goes undetected in hospitalized patients. Without treatment, it can prolong hospital stays, raise mortality risk, and worsen long-term outcomes. Until now, AI-driven delirium prediction models have struggled to demonstrate tangible improvements in patient care, say the investigators.
"The motivation behind our study at Mount Sinai was clear. Current AI-based delirium prediction models haven’t yet shown real-world benefits for patient care," said senior corresponding study author Joseph Friedman, MD, Founder and Director of Delirium Services for the Mount Sinai Health System and Professor of Psychiatry, and Neuroscience, at the Icahn School of Medicine at Mount Sinai. "We wanted to change that by creating a model that accurately calculates delirium risk in real time and integrates smoothly into clinical workflows, helping hospital staff catch and treat more patients with delirium who might otherwise be overlooked."
Rather than building an AI model in isolation and testing it later in hospitals, the research team worked closely with Mount Sinai clinicians and hospital staff from the start. This "vertical integration" approach allowed them to refine the model in real time, ensuring it was both effective and practical for clinical use.
When deployed at Mount Sinai, the AI model dramatically improved delirium detection, resulting in:
- A 400 percent increase in identified cases without increasing time spent screening patients
- Safer prescribing by reducing the use of potentially inappropriate medications in older adults
- Strong, reliable performance in a real-world hospital setting
In their study, which involved more than 32,000 patients admitted to The Mount Sinai Hospital in New York City, the researchers used the AI model to analyze a combination of structured data and clinicians’ notes from electronic health records. It used machine learning to identify chart data patterns associated with a high risk of delirium and applied natural language processing to identify patterns from the language of chart notes written by hospital staff. This approach captures staff observations of subtle mental status changes in patients who are delirious or at heightened risk. An individual staff member writing a note may be unaware at that time that their clinical observations are helping to improve the AI model’s accuracy.
Notably, the model was tested in a highly diverse patient population with a wide range of medical and surgical conditions—far broader than the narrow groups typically included in studies of machine learning-based delirium risk prediction models.
The tool significantly improved monthly delirium detection rates—from 4.4 to 17.2 percent—allowing for earlier intervention. Patients identified also received lower doses of sedative medications, potentially reducing side effects and improving overall care.
“Our model isn’t about replacing doctors—it’s about giving them a powerful tool to streamline their work,” says Dr. Friedman. “By doing the heavy lifting of analyzing vast amounts of patient data, our machine learning approach allows health care providers to focus their expertise on diagnosing and treating patients more effectively and with greater precision.”
While the AI model has delivered strong results at The Mount Sinai Hospital, and testing is underway at other Mount Sinai locations, validation will be needed at other hospital systems to evaluate its performance in different settings and adjust if needed.
“This research demonstrates the quantum leaps we are achieving by building AI-driven clinical decision support into hospital operations. We are improving patient safety and outcomes by bringing the right team to the right patient at the right time so patients receive specialized care tailored to their needs,” says study co-author David L. Reich MD, Chief Clinical Officer of the Mount Sinai Health System and President of The Mount Sinai Hospital. “To become a learning health system, we must continue this pathway of developing, testing, deploying, and fine-tuning AI-tools that are seamlessly integrated into health care workflows. Previously, we found that AI clinical decision support works in addressing malnutrition and clinical deterioration, where Mount Sinai’s use of real-time AI alerts to predict declining health, accelerated treatment and reduced hospital deaths.
The paper is titled “Machine Learning Multimodal Model for Delirium Risk Stratification.”
The study’s authors, as listed in the journal, are Joseph I. Friedman, MD; Prathamesh Parchure, MSC; Fu-Yuan Cheng, MS; Weijia Fu, MS; Satyanarayana Cheertirala, MS; Prem Timsina, ScD; Ganesh Raut, MS; Katherine Reina, DNP; Josiane Joseph-Jimerson, DNP; Madhu Mazumdar, PhD; Robert Freeman, DNP; David L. Reich, MD; and Arash Kia, MD.
About the Icahn School of Medicine at Mount Sinai
The Icahn School of Medicine at Mount Sinai is internationally renowned for its outstanding research, educational, and clinical care programs. It is the sole academic partner for the seven member hospitals* of the Mount Sinai Health System, one of the largest academic health systems in the United States, providing care to New York City’s large and diverse patient population.
The Icahn School of Medicine at Mount Sinai offers highly competitive MD, PhD, MD-PhD, and master’s degree programs, with enrollment of more than 1,200 students. It has the largest graduate medical education program in the country, with more than 2,600 clinical residents and fellows training throughout the Health System. Its Graduate School of Biomedical Sciences offers 13 degree-granting programs, conducts innovative basic and translational research, and trains more than 560 postdoctoral research fellows.
Ranked 11th nationwide in National Institutes of Health (NIH) funding, the Icahn School of Medicine at Mount Sinai is among the 99th percentile in research dollars per investigator according to the Association of American Medical Colleges. More than 4,500 scientists, educators, and clinicians work within and across dozens of academic departments and multidisciplinary institutes with an emphasis on translational research and therapeutics. Through Mount Sinai Innovation Partners (MSIP), the Health System facilitates the real-world application and commercialization of medical breakthroughs made at Mount Sinai.
-------------------------------------------------------
* Mount Sinai Health System member hospitals: The Mount Sinai Hospital; Mount Sinai Brooklyn; Mount Sinai Morningside; Mount Sinai Queens; Mount Sinai South Nassau; Mount Sinai West; and New York Eye and Ear Infirmary of Mount Sinai
About the Mount Sinai Health System
Mount Sinai Health System is one of the largest academic medical systems in the New York metro area, with 48,000 employees working across seven hospitals, more than 400 outpatient practices, more than 600 research and clinical labs, a school of nursing, and a leading school of medicine and graduate education. Mount Sinai advances health for all people, everywhere, by taking on the most complex health care challenges of our time—discovering and applying new scientific learning and knowledge; developing safer, more effective treatments; educating the next generation of medical leaders and innovators; and supporting local communities by delivering high-quality care to all who need it.
Through the integration of its hospitals, labs, and schools, Mount Sinai offers comprehensive health care solutions from birth through geriatrics, leveraging innovative approaches such as artificial intelligence and informatics while keeping patients’ medical and emotional needs at the center of all treatment. The Health System includes approximately 9,000 primary and specialty care physicians and 10 free-standing joint-venture centers throughout the five boroughs of New York City, Westchester, Long Island, and Florida. Hospitals within the System are consistently ranked by Newsweek’s® “The World’s Best Smart Hospitals, Best in State Hospitals, World Best Hospitals and Best Specialty Hospitals” and by U.S. News & World Report's® “Best Hospitals” and “Best Children’s Hospitals.” The Mount Sinai Hospital is on the U.S. News & World Report® “Best Hospitals” Honor Roll for 2025-2026.
For more information, visit https://www.mountsinai.org or find Mount Sinai on Facebook, Instagram, LinkedIn, X, and YouTube.