Teaching Preschool Caregivers about Healthy Behaviors May Promote Healthier Lifestyle in Some High-Risk Groups
Study Shows Vascular Ultrasounds and Adhering to Interventional Education in Underserved Communities can Improve Health among Parents and School Staff
A unique study conducted in a multi-ethnic, underserved community in New York City shows if young adults are properly taught about heart healthy behaviors and strictly adhere to specific interventions, they may see significant benefits to their cardiovascular health when compared to those who do not have any health education intervention, according to Mount Sinai researchers. Their findings also suggest that showing young adults ultrasound images of plaque in their arteries can provide helpful information to improve their cardiovascular health and their future lifestyle.
The study is part of an ambitious, multinational effort to intervene early in the lives of children so they can form a lifetime of heart healthy habits. These new results come after a highly successful intervention involving more than 500 preschoolers at 15 head start schools in the Harlem section of Manhattan, an urban area that is socioeconomically disadvantaged—a situation commonly linked to higher rates of obesity, heart disease, and other health issues. It showed students who went through a specialized health curriculum significantly improved their attitudes and behaviors about a healthy lifestyle, including diet, exercise and heart health.
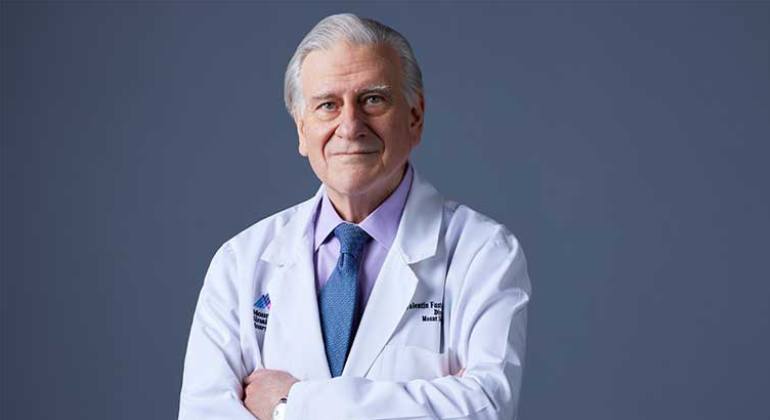
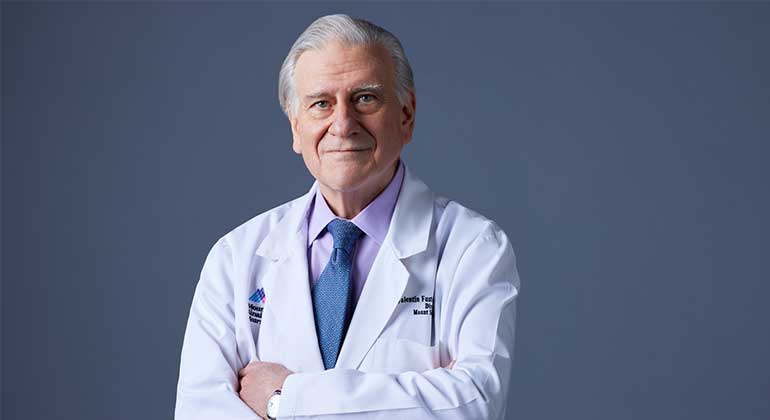
Researchers focused on caretakers of preschool students in those same Harlem schools (parents, family members, teachers and school staff). Valentin Fuster, MD, PhD, Director of Mount Sinai Heart and Physician-in-Chief of The Mount Sinai Hospital, created and led the trial, called the FAMILIA Project at Mount Sinai Heart. Results were published in the November 11 issue of the Journal of the American College of Cardiology and will be presented on November 17 during the American Heart Association’s Scientific Sessions 2019.
“The interventions applied to caretakers are easy to implement, and results show if adults follow and stick to simple education plans they may see positive results and reduce their risk factors for developing heart disease throughout their lives,” explained Dr. Fuster. “The FAMILIA project has already shown that early interventional health education is effective for preschoolers and the new results for caretakers further prove low-cost methods can promote health among parents and school staff. We hope in time we can integrate this project into schools across the country to help more families, especially those in underserved communities.”
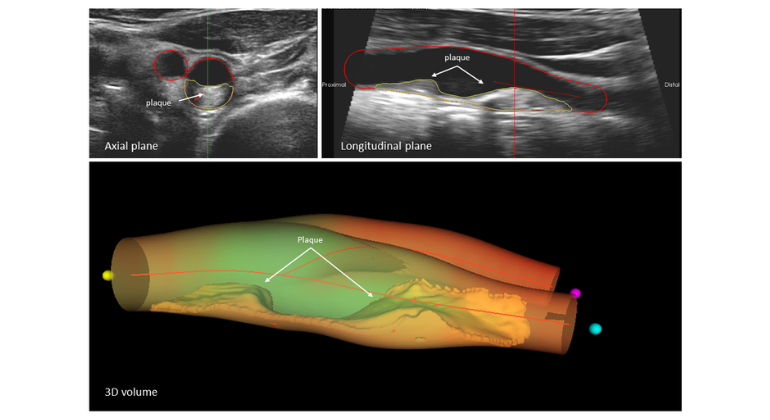
The FAMILIA team enrolled 635 preschool caregivers in 15 different Head Start schools in Harlem (average age 38 years old, 83 percent female, 57 percent Hispanic/Latino and 31 percent African-American). Harlem’s population is predominantly African American and Hispanic/Latino—groups that experience a higher risk of cardiovascular disease. One control group and two different intervention groups went through the program for approximately a 12-month period. Before the intervention began, researchers gave the adults an individualized health assessment that included measurements of weight, blood pressure, body mass index, lipid profile, and blood glucose. Caregivers also had vascular ultrasounds to determine if they had plaque in their arteries and received printed photos of those scans, along with handouts on heart health, controlling weight, and portion control.
All participants answered a comprehensive questionnaire before the study began to measure their knowledge, attitudes, and habits about their health. Questions addressed their nutrition, physical activity, tobacco use, alcohol consumption, if they have conditions such as heart disease or diabetes and a family history of health problems.
One intervention group went through an “Intensive Individual Intervention Program” (IIIP), where they had one-on-one counseling sessions with a trained lifestyle coach and followed a manual created by the FAMILIA team. Monthly coaching session topics included health and heart disease, eating habits, shopping for healthy food on a budget, cooking healthy, exercise, and stress management. Caregivers also got an activity-monitoring device to wear for tracking physical activity and provide motivation for exercise.
The other intervention group went through “Peer-to-Peer Program Intervention” (PPPI) where they went to monthly peer-led support group sessions. During each session, they followed a curriculum designed by the FAMILIA Team that focused on health and heart disease, eating habits, shopping for healthy food on a budget, cooking healthy, exercise, being active as a family and stress management.
Adults in the control group did not have a structured program. Instead, they received “Family Newsletters” (also handed out to intervention groups) that talked about diet and exercise and provided activities and at-home routines to follow with their children.
Researchers analyzed all participants 12 months after the study began and gave them the same health assessment with a vascular ultrasound. They used the validated Fuster-BEWAT Score (B-blood pressure, E-exercise, W-weight, A-Alimentation, T- Tobacco) to measure results. The overall BEWAT score ranges from zero (poor health) to 15 (ideal cardiovascular health). Baseline for participants was 9.3.
Results show caregivers who participated and strictly adhered to at least 50 percent of the curriculum had a greater and statistically significant change in their BEWAT Score compared to caregivers who went through less than half of it. Adults with high adherence improved scores by approximately 0.30 points from baseline at 12 months compared to low adherence caregivers. This data leads researchers to conclude that closely following lifestyle interventions may greatly improve health outcomes.
Another important finding was that caregivers in the intervention groups with evidence of atherosclerosis in vascular ultrasounds going into the study had the strongest results and most improvement following the intervention. Seeing pictures of their plaque and understanding what the images showed significantly boosted the interventional effects. Additionally, caretakers with a lower baseline score who had atherosclerosis at the start of the study benefitted the most from the intervention. Researchers conclude if caretakers learn they may have heart issues early on, early intervention could prevent them from having future cardiac events like heart attack and stroke.
At 12 months, both the control and intervention groups improved their BEWAT scores by an average of .20 points (modest change) from the baseline score of 9.3, mainly driven by higher exercise and blood pressure scores.
The FAMILIA team then evaluated participants again at 24 months, one year after stopping the intervention, but did not perform ultrasounds. Researchers observed caregivers with atherosclerosis at baseline and those who strongly participated in the intervention maintained healthier habits and had slightly higher BEWAT scores when compared to other caregivers in the interventional and control groups. They also found overall lack of intervention for the year led to similar BEWAT scores among plaque-free caregivers in the interventional and control groups.
FAMILIA follows other successful interventions in children and caregivers led by Dr. Fuster in Colombia and Spain, but FAMILIA is unique in being the first time the health promotion curriculum was family-based and implemented in a multi-ethnic, underprivileged urban population. Dr. Fuster and his team plan to expand the program across the five boroughs of New York City. This ambitious project will also evaluate how family socioeconomic status and teachers’ characteristics may affect the implementation and the efficacy of school-based health promotion programs.
The FAMILIA project was funded by a grant from the American Heart Association.
About the Mount Sinai Health System
Mount Sinai Health System is one of the largest academic medical systems in the New York metro area, with 48,000 employees working across seven hospitals, more than 400 outpatient practices, more than 600 research and clinical labs, a school of nursing, and a leading school of medicine and graduate education. Mount Sinai advances health for all people, everywhere, by taking on the most complex health care challenges of our time—discovering and applying new scientific learning and knowledge; developing safer, more effective treatments; educating the next generation of medical leaders and innovators; and supporting local communities by delivering high-quality care to all who need it.
Through the integration of its hospitals, labs, and schools, Mount Sinai offers comprehensive health care solutions from birth through geriatrics, leveraging innovative approaches such as artificial intelligence and informatics while keeping patients’ medical and emotional needs at the center of all treatment. The Health System includes approximately 9,000 primary and specialty care physicians and 10 free-standing joint-venture centers throughout the five boroughs of New York City, Westchester, Long Island, and Florida. Hospitals within the System are consistently ranked by Newsweek’s® “The World’s Best Smart Hospitals, Best in State Hospitals, World Best Hospitals and Best Specialty Hospitals” and by U.S. News & World Report's® “Best Hospitals” and “Best Children’s Hospitals.” The Mount Sinai Hospital is on the U.S. News & World Report® “Best Hospitals” Honor Roll for 2025-2026.
For more information, visit https://www.mountsinai.org or find Mount Sinai on Facebook, Instagram, LinkedIn, X, and YouTube.

Valentin Fuster, MD, PhD, Receives Prestigious Award from City of Barcelona, Spain
Jan 23, 2023 View All Press Releases
Samin Sharma, MD, Named Director of the Mount Sinai Cardiovascular Clinical Institute
Nov 28, 2022 View All Press Releases