AI System Finds Crucial Clues for Diagnoses in Electronic Health Records

Doctors often must make critical decisions in minutes, relying on incomplete information. While electronic health records contain vast amounts of patient data, much of it remains difficult to interpret quickly—especially for patients with rare diseases or unusual symptoms.
Now, researchers at the Icahn School of Medicine at Mount Sinai and collaborators have developed an artificial intelligence system, called InfEHR, that links unconnected medical events over time, creating a diagnostic web that reveals hidden patterns. Published in the September 26 online issue of Nature Communications, the study shows that Inference on Electronic Health Records (InfEHR) transforms millions of scattered data points into actionable, patient-specific diagnostic insights.
"We were intrigued by how often the system rediscovered patterns that clinicians suspected but couldn't act on because the evidence wasn't fully established," says senior corresponding author Girish N. Nadkarni, MD, MPH, Chair of the Windreich Department of Artificial Intelligence and Human Health, Director of the Hasso Plattner Institute for Digital Health, the Irene and Dr. Arthur M. Fishberg Professor of Medicine at the Icahn School of Medicine at Mount Sinai, and the Chief AI Officer of the Mount Sinai Health System. "By quantifying those intuitions, InfEHR gives us a way to validate what was previously just a hunch and opens the door to entirely new discoveries."
Most medical artificial intelligence (AI), no matter how advanced, applies the same diagnostic process to every patient. InfEHR works differently by tailoring its analysis to each individual. The system builds a network from a patient’s specific medical events and their connections over time, allowing it to not only provide personalized answers but also to ask personalized questions. By adapting both what it looks for and how it looks, InfEHR brings personalized diagnostics within reach, the investigators say.
In the study, InfEHR analyzed deidentified, privacy-protected electronic records from two hospital systems (Mount Sinai in New York and UC Irvine in California). The investigators turned each patient’s medical timeline—visits, lab tests, medications, vital signs—into a network that showed how events connected over time. The AI studied many of these networks to learn which combinations of clues tend to appear when a hidden condition is present.
With a small set of doctor-confirmed examples to calibrate it, the system checked whether it could correctly flag two real-world problems: newborns who develop sepsis despite negative blood cultures and patients who develop a kidney injury after surgery. Its performance in identifying patients with the diagnosis was compared with current clinical rules and validated across both hospitals. Notably, the system could also signal when the record lacked sufficient information, allowing it to respond “not sure” as a safety feature.
The study found that InfEHR can detect disease patterns that are invisible when examining isolated data. For neonatal sepsis without positive blood cultures—a rare, life-threatening condition—InfEHR was 12–16 times more likely to identify affected infants than current methods. For postoperative kidney injury, the system flagged at-risk patients 4–7 times more effectively. Importantly, InfEHR achieved this without needing large amounts of training data, learning directly from patient records and adapting across hospitals and populations.
“Traditional AI asks, ‘Does this patient resemble others with the disease?’ InfEHR takes a different approach: ‘Could this patient’s unique medical trajectory result from an underlying disease process?’ It’s the difference between simply matching patterns and uncovering causation,” says lead author Justin Kauffman, MS, Senior Data Scientist at the Windreich Department of Artificial Intelligence and Human Health at the Icahn School of Medicine.
Importantly, in addition, InfEHR flags how confident it is in its predictions. Unlike other AI that may give a wrong answer with certainty, InfEHR knows when to say, ‘I don’t know’—a key safety feature for real-world clinical use, say the investigators.
The team is making the coding of InfEHR available to other researchers as it continues to study uses of the system. For example, the team will next explore how InfEHR could personalize treatment decisions by learning from clinical trial data and extending those insights to patients whose specific characteristics or symptoms were not fully represented in the original trials.
“Clinical trials often focus on specific populations, while doctors care for every patient,” Mr. Kauffman says. “Our probabilistic approach helps bridge that gap, making it easier for clinicians to see which research findings truly apply to the patient in front of them.”
The paper is titled “InfEHR: Clinical phenotype resolution through deep geometric learning on electronic health records.” The study’s authors, as listed in the journal, are Justin Kauffman, Emma Holmes, Akhil Vaid, Alexander W. Charney, Patricia Kovatch, Joshua Lampert, Ankit Sakhuja, Marinka Zitnik, Benjamin S. Glicksberg, Ira Hofer, and Girish N. Nadkarni.
This work was supported in part by the National Institutes of Health grant UL1TR004419, and the Clinical and Translational Science Awards grant UL1TR004419 from the National Center for Advancing Translational Sciences. Research reported in this publication was also supported by the Office of Research Infrastructure of the National Institutes of Health under awards S10OD026880 and S10OD030463.
For more Mount Sinai artificial intelligence news, visit: https://icahn.mssm.edu/about/artificial-intelligence.
About Mount Sinai's Windreich Department of AI and Human Health
Led by Girish N. Nadkarni, MD, MPH—an international authority on the safe, effective, and ethical use of AI in health care—Mount Sinai’s Windreich Department of AI and Human Health is the first of its kind at a U.S. medical school, pioneering transformative advancements at the intersection of artificial intelligence and human health.
The Department is committed to leveraging AI in a responsible, effective, ethical, and safe manner to transform research, clinical care, education, and operations. By bringing together world-class AI expertise, cutting-edge infrastructure, and unparalleled computational power, the department is advancing breakthroughs in multi-scale, multimodal data integration while streamlining pathways for rapid testing and translation into practice.
The Department benefits from dynamic collaborations across Mount Sinai, including with the Hasso Plattner Institute for Digital Health at Mount Sinai—a partnership between the Hasso Plattner Institute for Digital Engineering in Potsdam, Germany, and the Mount Sinai Health System—which complements its mission by advancing data-driven approaches to improve patient care and health outcomes.
At the heart of this innovation is the renowned Icahn School of Medicine at Mount Sinai, which serves as a central hub for learning and collaboration. This unique integration enables dynamic partnerships across institutes, academic departments, hospitals, and outpatient centers, driving progress in disease prevention, improving treatments for complex illnesses, and elevating quality of life on a global scale.
In 2024, the Department's innovative NutriScan AI application, developed by the Mount Sinai Health System Clinical Data Science team in partnership with Department faculty, earned Mount Sinai Health System the prestigious Hearst Health Prize. NutriScan is designed to facilitate faster identification and treatment of malnutrition in hospitalized patients. This machine learning tool improves malnutrition diagnosis rates and resource utilization, demonstrating the impactful application of AI in health care.
For more information on Mount Sinai's Windreich Department of AI and Human Health, visit: ai.mssm.edu
About the Hasso Plattner Institute at Mount Sinai
At the Hasso Plattner Institute for Digital Health at Mount Sinai, the tools of data science, biomedical and digital engineering, and medical expertise are used to improve and extend lives. The Institute represents a collaboration between the Hasso Plattner Institute for Digital Engineering in Potsdam, Germany, and the Mount Sinai Health System.
Under the leadership of Girish Nadkarni, MD, MPH, who directs the Institute, and Professor Lothar Wieler, a globally recognized expert in public health and digital transformation, they jointly oversee the partnership, driving innovations that positively impact patient lives while transforming how people think about personal health and health systems.
The Hasso Plattner Institute for Digital Health at Mount Sinai receives generous support from the Hasso Plattner Foundation. Current research programs and machine learning efforts focus on improving the ability to diagnose and treat patients.
About the Icahn School of Medicine at Mount Sinai
The Icahn School of Medicine at Mount Sinai is internationally renowned for its outstanding research, educational, and clinical care programs. It is the sole academic partner for the seven member hospitals* of the Mount Sinai Health System, one of the largest academic health systems in the United States, providing care to New York City’s large and diverse patient population.
The Icahn School of Medicine at Mount Sinai offers highly competitive MD, PhD, MD-PhD, and master’s degree programs, with enrollment of more than 1,200 students. It has the largest graduate medical education program in the country, with more than 2,600 clinical residents and fellows training throughout the Health System. Its Graduate School of Biomedical Sciences offers 13 degree-granting programs, conducts innovative basic and translational research, and trains more than 560 postdoctoral research fellows.
Ranked 11th nationwide in National Institutes of Health (NIH) funding, the Icahn School of Medicine at Mount Sinai is among the 99th percentile in research dollars per investigator according to the Association of American Medical Colleges. More than 4,500 scientists, educators, and clinicians work within and across dozens of academic departments and multidisciplinary institutes with an emphasis on translational research and therapeutics. Through Mount Sinai Innovation Partners (MSIP), the Health System facilitates the real-world application and commercialization of medical breakthroughs made at Mount Sinai.
-------------------------------------------------------
* Mount Sinai Health System member hospitals: The Mount Sinai Hospital; Mount Sinai Brooklyn; Mount Sinai Morningside; Mount Sinai Queens; Mount Sinai South Nassau; Mount Sinai West; and New York Eye and Ear Infirmary of Mount Sinai
About the Mount Sinai Health System
Mount Sinai Health System is one of the largest academic medical systems in the New York metro area, with 48,000 employees working across seven hospitals, more than 400 outpatient practices, more than 600 research and clinical labs, a school of nursing, and a leading school of medicine and graduate education. Mount Sinai advances health for all people, everywhere, by taking on the most complex health care challenges of our time—discovering and applying new scientific learning and knowledge; developing safer, more effective treatments; educating the next generation of medical leaders and innovators; and supporting local communities by delivering high-quality care to all who need it.
Through the integration of its hospitals, labs, and schools, Mount Sinai offers comprehensive health care solutions from birth through geriatrics, leveraging innovative approaches such as artificial intelligence and informatics while keeping patients’ medical and emotional needs at the center of all treatment. The Health System includes approximately 9,000 primary and specialty care physicians and 10 free-standing joint-venture centers throughout the five boroughs of New York City, Westchester, Long Island, and Florida. Hospitals within the System are consistently ranked by Newsweek’s® “The World’s Best Smart Hospitals, Best in State Hospitals, World Best Hospitals and Best Specialty Hospitals” and by U.S. News & World Report's® “Best Hospitals” and “Best Children’s Hospitals.” The Mount Sinai Hospital is on the U.S. News & World Report® “Best Hospitals” Honor Roll for 2025-2026.
For more information, visit https://www.mountsinai.org or find Mount Sinai on Facebook, Instagram, LinkedIn, X, and YouTube.

AI Could Help Predict Nutrition Risks in ICU Patients, Study Finds
Dec 22, 2025 View All Press Releases
Adding a Lookup Step Makes AI Better at Assigning Medical Diagnosis Codes
Sep 25, 2025 View All Press Releases
Like Humans, AI Can Jump to Conclusions, Mount Sinai Study Finds
Jul 22, 2025 View All Press Releases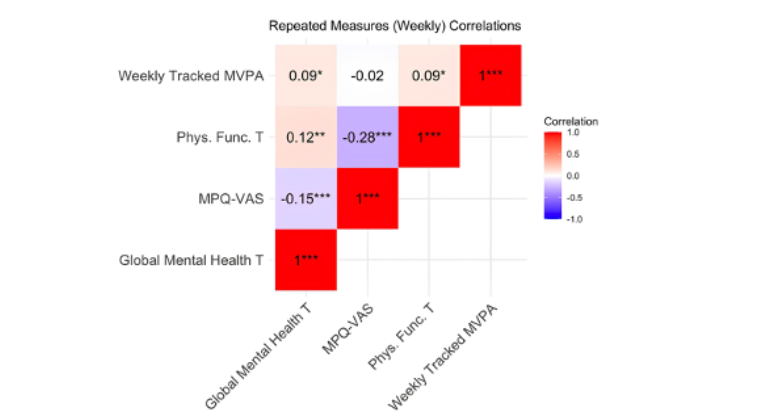
Physical Activity Boosts Mental Health in Women With Chronic Pelvic Pain Disorders
Feb 26, 2025 View All Press Releases