Study Reveals New Insights Into Immune System Role in Lung Cancer Risk
Immune-boosting strategies may prevent cancer in high-risk groups
Recent developments in cancer research have highlighted the vital role of the immune system, particularly in the notable successes of cancer immunotherapy.
Now, a paradigm-shifting study led by researchers at the Icahn School of Medicine at Mount Sinai in New York in collaboration with the University of Helsinki, Massachusetts General Hospital, and the Broad Institute of MIT and Harvard sheds light on how variations in immune genetics influence lung cancer risk, potentially paving the way for enhanced prevention strategies and screening.
The findings were described in the February 22 online issue of Science [DOI number: 10.1126/science.adi3808].
The investigators utilized genetic epidemiology and multimodal genomic analyses of data from the UK Biobank, validating it in FinnGen. Their study focused on human leukocyte antigen (HLA) molecules—the most diverse genes in the human genome and at the core of immune recognition. These genes contain instructions to make proteins, which play a crucial role in presenting foreign antigens on cell surfaces. This process aids the immune system in identifying and eliminating threats such as cancer cells.
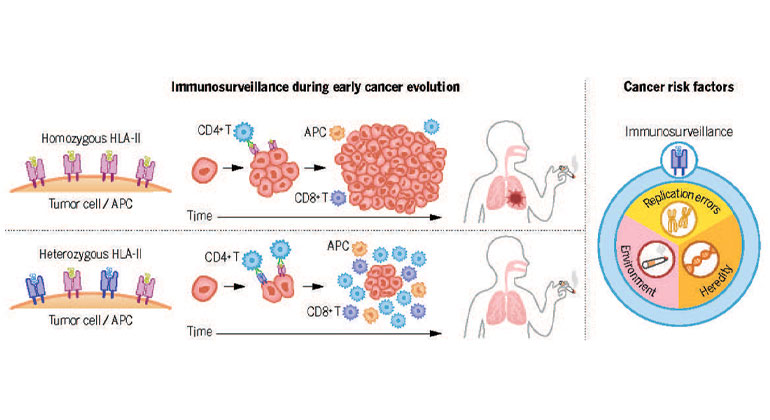
How does the immune system fight cancer? In smokers, having diverse HLA-II genes helps by presenting tobacco-related antigens, aiding in early cancer detection. Thus, genetic variation in immunosurveillance affects cancer risk. Krishna, et al., Science
Surprisingly, the study found that individuals with heterozygosity (having different versions of a gene) at HLA-II, rather than HLA-I, experienced a decreased risk of lung cancer. This effect was particularly pronounced among smokers, a population already at higher risk for lung cancer due to exposure to carcinogens.
"Our findings challenge conventional thinking by demonstrating that immune genetics, specifically HLA-II heterozygosity, plays a significant role in lung cancer risk, especially among smokers," says co-senior author Diego Chowell, PhD, Assistant Professor of Oncological Sciences, and Immunology and Immunotherapy at Icahn Mount Sinai. “Further, when we added polygenic risk scores—which is a measure of genetic predisposition based on multiple genes—to the analysis, it increased the lifetime risk of lung cancer, specifically in smokers who have identical versions of the HLA-II genes.
The implications of this research extend beyond lung cancer, offering a new perspective on cancer risk assessment, the researchers say. The conventional thinking on the causes of cancer is that the disease is caused by random mutations arising during DNA replication, inherited mutations, and environmental factors. The research showed that the immune system is also part of the etiology of cancer, Dr. Chowell says. By considering immune genetics alongside hereditary and environmental factors, the investigators’ aim to develop more effective prevention strategies, potentially harnessing the immune system to combat cancer.
"These results highlight a previously overlooked aspect of cancer risk assessment," says co-senior author Robert Samstein, MD, PhD, Assistant Professor of Radiation Oncology, and Immunology and Immunotherapy at Icahn Mount Sinai. "Our study marks a big step toward understanding the intricate interplay between the immune system and cancer risk. We hope that by identifying individuals with increased susceptibility based on their immune genetics, we can implement more targeted screening, prevention, and treatment strategies."
Next, the research team plans to delve deeper into the mechanisms underlying HLA heterozygosity's protective effects, with a focus on preclinical models of disease. Additionally, they aim to explore the role of non-classical CD4 T cells and HLA class II in cancer biology, opening the door for potential progress in the mitigation and treatment of cancer.
The paper is titled “An immunogenetic basis for lung cancer risk.”
The remaining authors of the paper, all with Icahn Mount Sinai except where indicated, are: Chirag Krishna, PhD (a scientist at Pfizer, formerly with the Broad Institute of MIT & Harvard); Anniina Tervi, PhD (University of Helsinki); Miriam Saffern (PhD candidate); Eric A. Wilson, PhD; Seong-Keun Yoo, PhD; Nina Mars, MD, PhD (University of Helsinki and the Broad Institute of MIT and Harvard); Vladimir Roudko, PhD; Byuri Angela Cho, PhD; Samuel Edward Jones, PhD (University of Helsinki); Natalie Vaninov (PhD candidate); Myvizhi Esai Selvan, PhD; Zeynep H Gümüs, PhD; FinnGen Consortium; Tobias L. Lenz, PhD (University of Hamburg); Miriam Merad, MD, PhD; Paolo Boffetta, MD (Stony Brook University in New York and University of Bologna); Francisco Martínez-Jiménez, PhD (Stony Brook University in New York and Vall d’Hebron Institute of Oncology, Barcelona); and Hanna M. Ollila, PhD (Massachusetts General Hospital, Harvard Medical School, the Broad Institute of MIT and Harvard, and University of Helsinki).
Please see Science [DOI number: 10.1126/science.adi3808] to view details on funding and competing interests.
More information, including a copy of the paper, can be found online at the Science press package at https://www.eurekalert.org/press/scipak/.
About UK Biobank
UK Biobank is a large-scale biomedical database and research resource containing anonymised genetic, lifestyle and health information from half a million UK participants. UK Biobank’s database, which includes blood samples, heart and brain scans and genetic data of the volunteer participants, is globally accessible to approved researchers who are undertaking health-related research that’s in the public interest. UK Biobank’s resource was opened for research use in April 2012. Since then, 30,000 researchers from 100 countries have been approved to use it and more than 6,000 peer-reviewed papers that used the resource have now been published. You can find out more about UK Biobank at http://www.ukbiobank.ac.uk
About the Mount Sinai Health System
Mount Sinai Health System is one of the largest academic medical systems in the New York metro area, with 48,000 employees working across seven hospitals, more than 400 outpatient practices, more than 600 research and clinical labs, a school of nursing, and a leading school of medicine and graduate education. Mount Sinai advances health for all people, everywhere, by taking on the most complex health care challenges of our time—discovering and applying new scientific learning and knowledge; developing safer, more effective treatments; educating the next generation of medical leaders and innovators; and supporting local communities by delivering high-quality care to all who need it.
Through the integration of its hospitals, labs, and schools, Mount Sinai offers comprehensive health care solutions from birth through geriatrics, leveraging innovative approaches such as artificial intelligence and informatics while keeping patients’ medical and emotional needs at the center of all treatment. The Health System includes approximately 9,000 primary and specialty care physicians and 10 free-standing joint-venture centers throughout the five boroughs of New York City, Westchester, Long Island, and Florida. Hospitals within the System are consistently ranked by Newsweek’s® “The World’s Best Smart Hospitals, Best in State Hospitals, World Best Hospitals and Best Specialty Hospitals” and by U.S. News & World Report's® “Best Hospitals” and “Best Children’s Hospitals.” The Mount Sinai Hospital is on the U.S. News & World Report® “Best Hospitals” Honor Roll for 2025-2026.
For more information, visit https://www.mountsinai.org or find Mount Sinai on Facebook, Instagram, LinkedIn, X, and YouTube.