Diverticulitis
Diverticula are small, bulging sacs or pouches that form on the inner wall of the intestine. Diverticulitis occurs when these pouches become inflamed or infected. Most often, these pouches are in the lower part of the large intestine (colon).
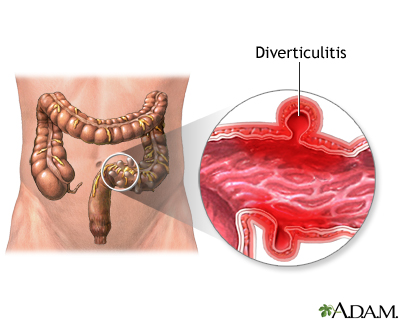
In most patients with diverticulosis, the diverticula do not cause any problems or symptoms. In some cases, a small, hard piece of stool is trapped in the opening of the diverticula, which then become inflamed. When this occurs, the condition is called diverticulitis. A small tear may develop in the lining of the intestine inside the diverticula, which can lead to an infection at the site and sometimes death of the segment of colon containing the diverticula.
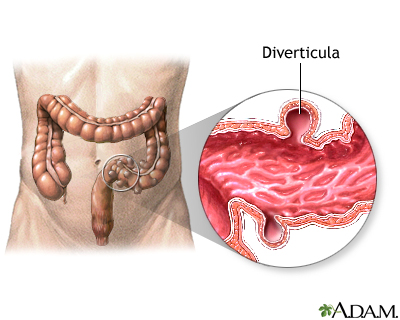
Diverticulosis occurs when small bulging sacs or pouches, called diverticula, form on the inner wall of the intestine. Most often, diverticula form in the large intestine (colon), but they may also occur in the in the jejunum in the small intestine. In most cases, diverticula cause no symptoms. In a small percentage of patients, diverticula can cause problems if they become inflamed or if they bleed.
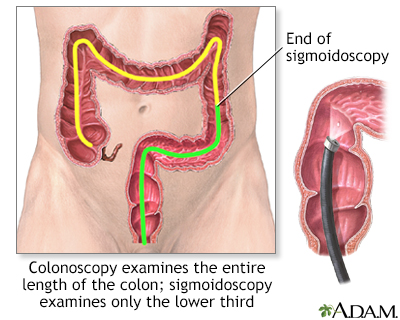
There are 3 basic tests for colon cancer; a stool test (to check for blood), sigmoidoscopy (inspection of the lower colon), and colonoscopy (inspection of the entire colon). All 3 are effective in catching cancers in the early stages, when treatment is most beneficial.
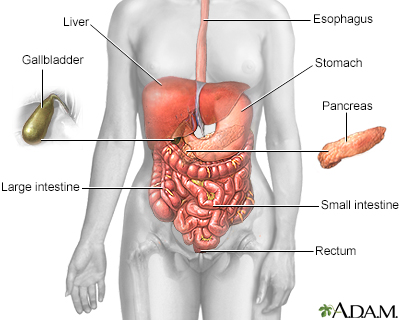
The esophagus, stomach, large and small intestine, aided by the liver, gallbladder and pancreas convert the nutritive components of food into energy and break down the non-nutritive components into waste to be excreted.
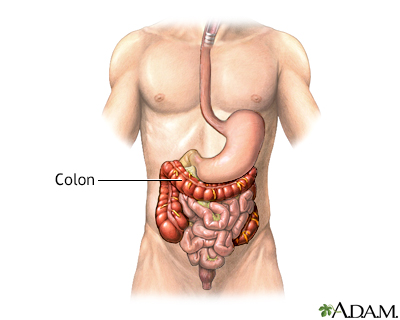
The colon, or large intestine, is a muscular tube that begins at the end of the small intestine and runs to the rectum. The colon absorbs water from liquid stool that is delivered to it from the small intestine.
Causes
The formation of pouches or sacs on the intestinal lining is called diverticulosis. It is found in more than half of Americans over age 60. However, no one knows exactly what causes the pouches to form.
Eating a low-fiber diet mostly made up of processed foods may be a cause. Constipation and hard stools are more likely when you do not eat enough fiber. Straining to pass stools increases the pressure in the colon or intestines, which may lead to the formation of these pouches.
In some cases, one of the pouches can become inflamed and a small tear develops in the lining of the intestine. This can lead to an infection at the site. When this occurs, the condition is called diverticulitis. The cause of diverticulitis is not known.
Symptoms
People with diverticulosis often have no symptoms, but they may have bloating and cramping in the lower part of the belly. Rarely, they may notice blood in their stool or on toilet paper.
Symptoms of diverticulitis are more severe and often start suddenly, but they may become worse over a few days. They include:
- Tenderness, usually in the left lower part of the abdomen
- Bloating or gas
- Fever and chills
- Nausea and vomiting
- Not feeling hungry and not eating
Exams and Tests
Your health care provider will examine you. You may need blood tests to see if you have an infection.
Other tests that help diagnose diverticulitis may include:
- CT scan
- Ultrasound of the abdomen
- X-rays of the abdomen
Treatment
The treatment of diverticulitis depends on how serious the symptoms are. Some people may need to be in the hospital, but most of the time, the problem can be treated at home.
To help with the pain, your provider may suggest that you:
- Rest in bed and use a heating pad on your belly.
- Take pain medicines (ask your provider which ones you should use).
- Drink only fluids for a day or two, and then slowly begin drinking thicker liquids and then eating foods.
The provider may treat you with antibiotics.
After you are better, your provider will suggest that you add more fiber to your diet. Eating more fiber can help prevent future attacks. If you have bloating or gas, reduce the amount of fiber you eat for a few days.
Once these pouches have formed, you will have them for life. Diverticulitis can return, but some providers think a high-fiber diet may lessen your chances of a recurrence.
Outlook (Prognosis)
Most often, this is a mild condition that responds well to treatment. Some people will have more than one attack of diverticulitis. Surgery may be needed in some cases. Many times, providers will recommend that you have a colonoscopy after diverticulitis has healed. This can help to rule out other conditions that could mimic diverticulitis symptoms.
Possible Complications
More serious problems that may develop are:
- Abnormal connections that form between parts of the colon or between the colon and another part of the body (fistula)
- Hole or tear in the colon (perforation)
- Narrowed area in the colon (stricture)
- Pocket filled with pus or infection (abscess)
- Bleeding from the diverticula
When to Contact a Medical Professional
Contact your provider if symptoms of diverticulitis occur.
Also call if you have diverticulitis and you have:
- Blood in your stools
- Fever above 100.4°F (38°C) that does not go away
- Nausea, vomiting, or chills
- Sudden belly or back pain that gets worse or is very severe
References
Bhuket TP, Stollman NH. Diverticular disease of the colon. In: Feldman M, Friedman LS, Brandt LJ, eds. Sleisenger and Fordtran's Gastrointestinal and Liver Disease. 11th ed. Philadelphia, PA: Elsevier; 2021:chap 121.
Kuemmerle JF. Inflammatory and anatomic diseases of the intestine, peritoneum, mesentery, and omentum. In: Goldman L, Schafer AI, eds. Goldman-Cecil Medicine. 26th ed. Philadelphia, PA: Elsevier; 2020:chap 133.
Version Info
Last reviewed on: 5/4/2022
Reviewed by: Michael M. Phillips, MD, Emeritus Professor of Medicine, The George Washington University School of Medicine, Washington, DC. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.
