Dean’s Quarterly
The Icahn School of Medicine at Mount Sinai is a national and international leader in biomedical education, research, and patient care.
Dean’s Quarterly
The Dean's Quarterly report features the latest news and research from Icahn School of Medicine at Mount Sinai.
This report highlights:
- Addiction Institute Explores Effective Therapies
- A Transformational New Capital Campaign Is Under Way
- Rebuilding the Patient Experience From the Ground Up
- Mount Sinai Expands Research Into Environmental Exposures
- Mount Sinai Surgeons Advance a Promising New Technique That Treats the Most Devastating Form of Stroke
- Mount Sinai and the United Nations Collaborate on New Program to Improve Health Outcomes in the United States
- Detailed Studies of the Immune System
- Mount Sinai Surgeons Pioneer HIV-Positive Kidney Transplants
- New Appointments
Addiction Institute Explores Effective Therapies
The Icahn School of Medicine at Mount Sinai recently opened a new Addiction Institute that will address one of the nation’s greatest health concerns by exploring effective treatments for patients with substance abuse problems.
“Bringing science to bear on the development of new therapies has reached the top of the national agenda, and that is where Mount Sinai excels,” says Yasmin Hurd, PhD, the Ward-Coleman Chair in Translational Neuroscience and Director of the Addiction Institute at Mount Sinai.
The Institute will manage therapies for all types of substance abuse. By removing the traditional silos that separate research and clinical care, and unifying all areas of addiction under one umbrella, Dr. Hurd says the Institute is “well positioned to meet the challenges of New York City and the nation.” The Institute will leverage Mount Sinai’s considerable body of research and clinical expertise in neuroscience and behavioral health in order to move the field forward.
According to the 2016 U.S. Surgeon General’s Report on Alcohol, Drugs, and Health, more than 20 million Americans have substance abuse disorders and 12.5 million have reported misusing prescription painkillers. Despite decades of expense and effort focused on a criminal justice-based model for addressing substance-related problems, the report acknowledged that addiction remains a public health crisis with economic consequences in crime, health, and lost productivity totaling more than $400 billion annually. Dr. Hurd says the Institute’s collaboration with Mount Sinai’s other specialties such as precision medicine, population health, infectious disease, epidemiology, and genomics will help advance treatments and novel discoveries.
“The Institute’s modernized structure across a large, integrated health system will enable us to approach addiction in a cohesive way,” says Dr. Hurd. “In addition to prioritizing our research based on clinical needs, we want to understand the populations at risk and their patterns of behavior. Addiction is complex and one group cannot do it alone.”

An important aspect of the Institute’s work will be dispelling the stigma associated with addiction through greater understanding of the biological and behavioral complexities of substance use disorders. Another goal will be encouraging young clinicians to enter residencies and fellowships in the fields of addiction psychiatry and addiction medicine.
“We want to train the best and the brightest through enhanced clinical and research rigor to elevate the field,” says Dr. Hurd. “Clinical treatments for some addictions have not advanced in 50 years. This and other stigmas can deter young physicians from going into this field. Unless we improve the clinical toolkit available for clinicians we will not be able to change the trajectory of care.”
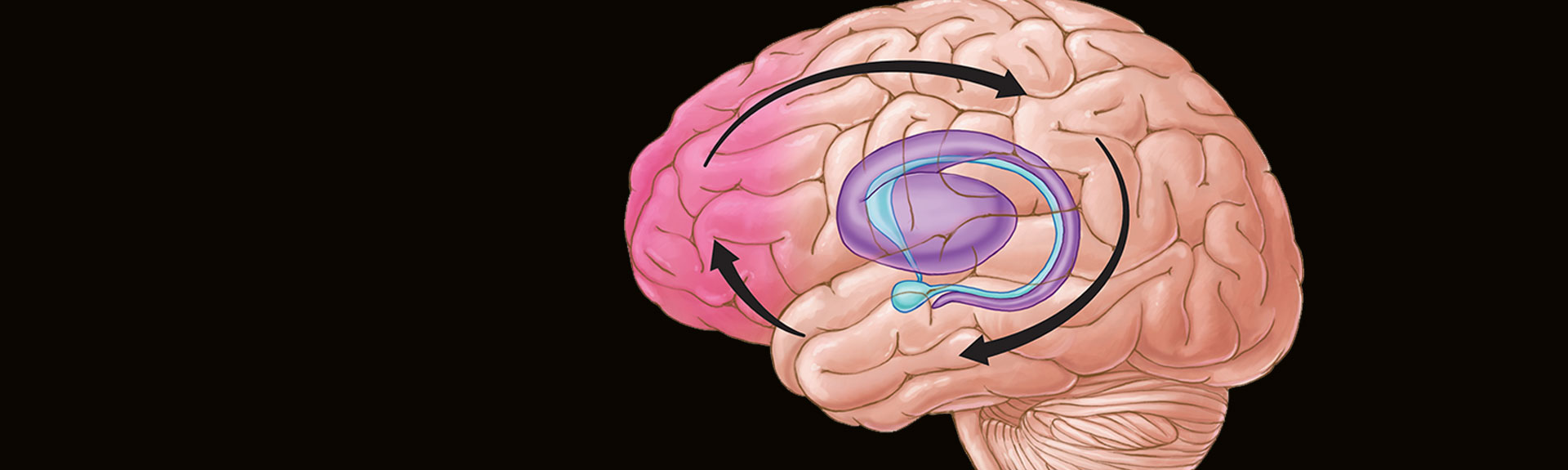
Decades of scientific studies have established that chronic substance misuse leads to profound disruptions of brain circuits involved in pleasure, reward, habit formation, stress, and decision-making. Repeated drug use alters the expression of genes to ultimately increase or decrease their production of proteins, leading to long-term changes in cellular function and even reshaping of the physical structure of neurons.
“Drugs can change the morphology of cells and induce a cascade of adverse events in the brain,” says Dr. Hurd. The Institute plans to move forward with multiple clinical trials that seek to reverse those disruptions. “Most addicts do not want to be addicted,” she adds. “Addiction can be treated. We need medical therapies that partner with behavioral therapies, and we need to be diverse in our treatment portfolio.”
A Transformational New Capital Campaign Is Under Way
The Mount Sinai Health System has launched a new capital campaign that is expected to raise $1.5 billion over the next seven years and serve as our roadmap for the future in medical research, patient care, and education.

As fundraising begins in earnest in 2018, we will steer a course that calls for significant investments in precision medicine, next-generation health care, and emerging areas in cancer, immunology, neuroscience, heart disease, and pediatrics. We will expand the scope of our clinical care in diabetes, obesity, kidney, lung, and gastrointestinal disease.
In addition, Mount Sinai will leverage its large and diverse patient population by establishing five institutes devoted to research in drug addiction; and environmental, adolescent, and women’s health; and creating breakthrough clinical trials.
Our new strategic plan was the result of a yearlong study led by myself and Eric J. Nestler, MD, PhD, Dean for Academic and Scientific Affairs, Director of The Friedman Brain Institute, and Nash Family Professor of Neuroscience. We enlisted 200 faculty members and more than 150 external experts—some of the best minds in science and medicine—to participate in a dynamic exchange of knowledge and ideas and help us chart our future in education, biomedical science, and clinical research.
The new campaign is based on their bold recommendations. It will be a first for the Mount Sinai Health System, which was formed in 2013 when The Mount Sinai Hospital, Mount Sinai Queens, and the Icahn School of Medicine at Mount Sinai combined with the former Continuum Health Partners and its five hospitals to become one of the largest health systems in the New York region.
We expect this campaign to be a game changer the way our campaign for The Mount Sinai Hospital and the Icahn School of Medicine was 10 years ago, when we raised $1.6 billion and created 19 research institutes, recruited 150 academic faculty, and established the 500,000-square-foot Leon and Norma Hess Center for Science and Medicine.
At that time, we entered into educational and industry partnerships that broadened our culture of innovation and entrepreneurship. We concentrated on high-performance computing, genomics, and multiscale biology, and advanced Mount Sinai’s research portfolio, which led to significant growth in funding for genetics, microbiology, pharmacology, and neurosciences from the National Institutes of Health. In addition, The Tisch Cancer Institute expanded its programs and became a National Cancer Institute-designated cancer center.
Rebuilding the Patient Experience From the Ground Up
What will the practice of medicine look like in 2025? That question is being explored by 35 biomedical researchers and data scientists at the Institute for Next-Generation Healthcare, a new initiative at the Icahn School of Medicine at Mount Sinai, with headquarters in New York City, and a satellite office in Silicon Valley.
The Institute’s mission is to find ways to improve the patient’s clinical experience through the use of smart software and artificial intelligence. In the process, the researchers are upending the way medical care has been delivered for decades, starting with primary care and moving on to specialties over time.

“Health care innovation has tried to shoehorn itself into a system that has largely been unchanged for 100 years,” says Joel Dudley, PhD, Director of the Institute for Next-Generation Healthcare. “Our Institute is throwing convention out the window. Knowing all the technologies that are available today, we’re asking ourselves, ‘how would we rebuild the patient experience, the clinical experience, from the ground up?’”
Replacing legacy medicine with digital medicine will enable the Institute to provide patients with quicker and more comprehensive test results and greater insight into their health. Moreover, patients and their physicians will be able to track disease progression over time so that lifestyle modifications and medical treatments can be introduced earlier and followed with greater precision, yielding better results.
Think of Uber and Airbnb, two major disruptors within their respective industries. “They are powered by software,” Dr. Dudley says. “This is analogous to what we’re trying to do with health care, at least with regard to primary care and screenings. It’s about how we bring health care to wherever the patient is in a way that is most convenient for them, and having it all managed by new types of intelligent software.”
The Institute’s new health care delivery location—scheduled to open on the Icahn School of Medicine campus in the fall—is being built as a prefabricated structure by Black Egg, an innovative experiential design studio. Black Egg has created high-tech spaces for pop stars and companies that include Google and Samsung Group.
No precursor to this facility currently exists. When all of the technology is built into the shell structure it will be moved to a space within Mount Sinai.
“The design is completely ours,” says Dr. Dudley. “We think the future is about a smarter, smaller footprint that is configurable, a scalable space, not a huge medical building. There’s no electronic program to support this. We’re creating it.”
Interestingly, as the actual clinical footprint shrinks, the amount of information that is gathered will grow exponentially. Wearable technology that collects patient information leading up to a checkup or immediately following one and provides deep baseline assessments also will play a large role in new health care delivery, along with 3D body scans that have sharply tuned metrics. A patient’s mental cognition and emotional state also will be monitored, as well as his or her genetic profile and gut microbiome information.
“No amount of information is too much for us,” Dr. Dudley says. “We are identifying domains of a patient’s physiology over time. What defines a normal, healthy person and how do you maintain that? No one actually knows. Right now we define health as the absence of disease and that’s an archaic way of looking at it.”
Since there is no electronic health program that supports the collection and analysis of this information, the Institute is building one that understands genetics and proteomics, and can provide patients and physicians with intuitive, actionable insights. The Institute is also creating software that lets patients control their own health information so they can personally evaluate whether certain interventions are working. Ultimately, the software would capture patient information in a structured way and build a body of evidence for each patient.
Mount Sinai Expands Research Into Environmental Exposures

Two international leaders in environmental health, husband and wife, Robert O. Wright, MD, MPH, and Rosalind J. Wright, MD, MPH, recently established the Institute for Exposomic Research at the Icahn School of Medicine at Mount Sinai. The Institute, the first in the world to focus on exposomics, will study the effects of environmental exposures on health and will translate these findings into new strategies for prevention and treatment.
“The exposome is a new research field and is analogous to genomics,” says the Institute’s Director, Dr. Robert Wright, the Ethel H. Wise Professor and Chair, Department of Environmental Medicine and Public Health, and Director, Senator Frank R. Lautenberg Environmental Health Sciences Laboratory. “While genomics concerns all the genetic factors that predict health, the exposome encompasses all the environmental factors that affect your health, including nutrition, social factors, chemicals, and the physical environment, from the time you are conceived until the time you die.”
Dr. Rosalind Wright, the Horace W. Goldsmith Professor in Children’s Health Research and Dean of Translational Biomedical Sciences at the Icahn School of Medicine, is the Institute’s Co-Director. The Wrights and their researchers will build upon the expertise of Mount Sinai’s existing Lautenberg Laboratory to develop new technologies and methodologies in exposomics.

Mount Sinai’s recent investment in the field has already led to significant funding from the National Institutes of Health (NIH), including a $9 million grant in December for Environmental influences on Child Health Outcomes (ECHO), to investigate the effects of a broad range of environmental exposures on children’s long-term health, and two additional $10 million NIH grants for the Children’s Health Exposure Analysis Resource (CHEAR) program. CHEAR provides laboratory resources to measure environmental chemicals, metabolites, hormones, and other factors representing components of the human exposome.
A major part of the CHEAR facilities’ mission will be analyzing the samples collected by ECHO, a seven-year study of 50,000 children followed longitudinally across the United States. Mount Sinai belongs to a consortium that includes programs in Boston and Virginia and will recruit 5,000 of these subjects. The Wrights are part of the committees now setting up protocols for the national ECHO study.
The new Institute will expand exposomics into research programs in disciplines across the Mount Sinai campus, including personalized medicine, cancer, women’s health, aging, immunology, and clinical trials.
Mount Sinai Surgeons Advance a Promising New Technique That Treats the Most Devastating Form of Stroke
Spontaneous bleeding in the brain, known as intracerebral hemorrhage (ICH), remains the least treatable and most devastating form of stroke. While it accounts for only 15 percent of all strokes, it is a leading cause of mortality, morbidity, and disability worldwide, and few effective treatment options exist.
Over recent months, however, Mount Sinai physicians have taken a leading national role in creating and implementing a new minimally invasive technique that is showing promise. ICH occurs when a small artery in the brain leaks blood directly into surrounding tissue and forms a localized hematoma (clot), which continues to destroy neurons and causes life-threatening pressure on the brain. Loss of balance, blurry vision, and difficulty speaking are among the common symptoms, as well as headache and vomiting, which increase gradually over minutes to hours.

The effort is being led by J Mocco, MD, MS, Director of the Cerebrovascular Center at the Mount Sinai Health System, and Professor and Vice Chair for Education in the Department of Neurosurgery at the Icahn School of Medicine at Mount Sinai, and Christopher Kellner, MD, Director of the Intracerebral Hemorrhage Program at Mount Sinai and Assistant Professor of Neurosurgery.
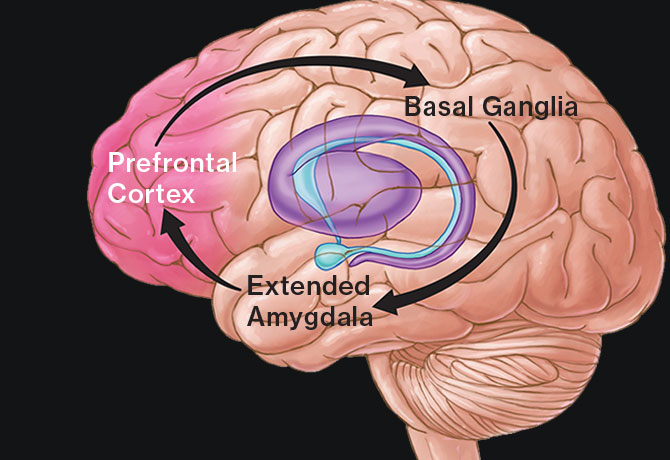
Over the course of 15 months, they have treated nearly 50 patients with a novel strategy to evacuate blood clots using ultrasound imaging, paired with intraoperative CT scanning and MRI-guided navigation, to precisely locate the blood clot within the brain. Through a tiny hole in the skull, a sheath containing a camera and an experimental suction device, known as the Apollo™ System, is navigated to the clot. The physicians then aspirate the clot with the Apollo device, normalizing the brain pressure.
In 2016, Dr. Mocco was named co-principal investigator of a Phase I clinical trial that will enroll approximately 50 patients at 10 sites across the United States to test the feasibility, safety, and efficacy of this procedure when compared to previously published standards. The trial, called the INVEST trial, is funded by Penumbra, Inc., the company that developed the Apollo System.
“We have just completed a six-month follow-up for the first 28 patients treated with this device, and although the data are preliminary, it appears that patients overall are doing very well with this procedure,” says Dr. Mocco.
One recent patient—an extremely active 86-year-old classical pianist—presented to
Mount Sinai Beth Israel in February.
“He came in with left arm and leg paralysis, slurred speech, and lethargy,” says Dr. Kellner. A CT scan revealed a very large 85 cc hemorrhage, and he was transferred to the Intracerebral Hemorrhage Center at Mount Sinai West. Given his age, and the size and the location of the hemorrhage, he scored a “4” on the ICH Score, which predicts a 97 percent chance of mortality within 30 days. The physicians removed the clot within 24 hours of the hemorrhage.
“He has made a remarkable recovery,” says Dr. Kellner. “He was discharged to the rehabilitation unit at The Mount Sinai Hospital after only 10 days. Currently, he is cognitively almost back to normal, can walk with a walker, and is back to playing the piano.”
Mount Sinai and the United Nations Collaborate on New Program to Improve Health Outcomes in the United States
The United States spends more money on health care than any other country, yet has poorer outcomes with shorter average life expectancies (78.8 years) than peer nations. Furthermore, a child born in poverty in Detroit has a life expectancy that is six years shorter than a child born in similar circumstances in New York City. And someone born on the Upper East Side of Manhattan has a life expectancy that is nine years longer than a person born 10 blocks away in East Harlem.
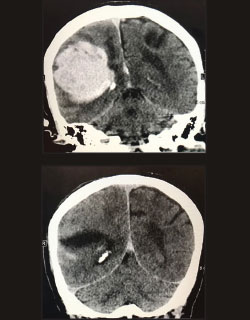
Mending this uneven patchwork of U.S. health outcomes will require a new model of care that embraces the use of community health workers (CHWs), nonclinical workers who provide underserved patients with the continuum of care they need, according to a new report from The Arnhold Institute for Global Health at the Icahn School of Medicine at Mount Sinai and the Office of the UN Secretary General’s Special Envoy for Health in Agenda 2030 and for Malaria. The report recommends creating a pilot program in Newark, New Jersey, a city with many non-English speaking residents that lags behind the rest of the state in health outcomes.
CHWs come from the same communities as their patients and enable patients to live healthier lives. They can serve as educators, for example, explaining the relationship between diabetes, blood sugar, high-sugar foods, and insulin in a way patients understand, or link patients to neighborhood exercise groups or food pantries that provide health-conscious meals. Such programs have been successful in South America, sub-Saharan Africa, and Southeast Asia.
“A growing body of evidence tells us that social, economic, genomic, and cultural factors can impact an individual’s ability to build and maintain health, and community health workers have the ability to help bridge that gap between medical advice and a patient’s ability to comply,” says Prabhjot Singh, MD, PhD, Director of The Arnhold Institute for Global Health, and the report’s senior author. Dr. Singh co-founded the One Million Community Health Worker Campaign with Jeffrey Sachs, PhD, an author and well-regarded sustainable development leader, whom The Arnhold Institute for Global Health is hosting as a visiting fellow through 2018.
Claire Qureshi, MBA, Vice President of Frontline Delivery, Office of the UN Secretary General’s Special Envoy for Health in Agenda 2030 and for Malaria, co-wrote the report with Dr. Singh. “We’ve seen the health impact and economic value of CHWs in countries around the world and fundamentally believe that working with them as part of integrated primary care is a better way to practice medicine,” says Ms. Qureshi. “With careful construction of the right care models, including the organizational and financial infrastructure needed to support them, CHWs can contribute enormously to patients, communities, and health systems alike.”
While CHWs have existed in the United States for decades, they have struggled to gain widespread acceptance. The services they provide have not been reimbursed by public or private health insurance plans. But, the report says, a renewed emphasis on keeping people healthy is creating the need for sustainable CHW programs to emerge.
Detailed Studies of the Immune System
For years, the endpoint that defined whether a cancer treatment was successful was the patient’s survival. Today, Mount Sinai’s researchers are able to understand how a treatment is working on a cellular and molecular level, with the support of the Human Immune Monitoring Core (HIMC), which also analyzes hundreds of preclinical and patient samples from academic medical centers throughout the New York City area.
The HIMC runs one of the nation’s largest full-service mass cytometry programs, providing researchers and clinicians with the extensive scientific and technical expertise that allows them to leverage a wide range of powerful technology platforms for detailed studies of the immune system.
What sets the HIMC apart from similar centers around the country is the level of support provided by the Core’s staff. Working closely with researchers, the HIMC team helps them understand the underlying basis for disease and guides them with the development of new and improved immune therapies.

Joshua Brody, MD, Assistant Professor of Medicine (Hematology and Medical Oncology), used the Core when he tested a unique in-situ vaccine for low-grade B-cell lymphoma that was aimed at increasing the number of dendritic cells. Dr. Brody collected blood samples from his patients during their treatments and provided them to the HIMC to perform in-depth analyses of their immune cells. Using a CyTOF2 machine—which is able to analyze 40 biomarkers on millions of individual cells in a single sample and pinpoint those that are particularly interesting—the HIMC team was able to show Dr. Brody that the treatment was working.
The team also explained how the treatment was affecting his patients’ dendritic cells and other immune cells. “We saw the confirmed effect of increased dendritic cells in the patients’ blood,” says Sacha Gnjatic, PhD, Associate Professor, Medicine (Hematology and Medical Oncology), who is also the HIMC’s Co-Director with Miriam Merad, MD, PhD, Professor of Oncological Sciences, and Medicine (Hematology and Medical Oncology).
“It’s hard to make a jigsaw puzzle if you can’t see the pieces,” says Dr. Brody. “The higher resolution of the CyTOF2 draws a whole picture. It offers us a way of validating the mechanism of these immunotherapies.”
Mount Sinai Surgeons Pioneer HIV-Positive Kidney Transplants
The Mount Sinai Hospital became the first hospital in New York State and the second in the nation to perform a kidney transplant from an HIV-positive deceased donor to an HIV-positive recipient last year, the result of federal legislation in 2015 that made such transplants possible.
Led by Sander Florman, MD, Director of the Recanati/Miller Transplantation Institute, and the Charles Miller, MD Professor of Surgery, Mount Sinai was one of only a few medical centers in the country with federal approval to perform liver and kidney transplants under the HIV Organ Policy Equity (HOPE) Act.

“The new law is a win-win for everyone,” says Dr. Florman. “This represents the potentially largest increase to the organ donor pool in many years and could provide more organs for everyone. The need for organs for transplantation far exceeds the availability, and the waiting lists continue to grow. People’s lives depend on these efforts so we must find ways to increase the donor supply and also encourage living donation.”
Prior to the HOPE Act, organs from HIV-positive donors were not legally allowed to be procured for transplant into patients with HIV— the only people eligible to receive them—which made organ waiting lists longer for all patients, including those without HIV.
Alexandra Harry, the first Mount Sinai patient to receive a kidney under the new law, called the transplant “a gift that has given me the opportunity for a better quality of life.” Since 2005, she had been on peritoneal dialysis, which had to be performed 10 hours each night. Ms. Harry says she learned about her eligibility to participate in Mount Sinai’s program only two weeks before she actually received a suitable kidney, so the entire process was very quick.
A few days after her surgery Ms. Harry said she felt “improvement almost immediately.” Her surgeon was Susan Lerner, MD, Assistant Professor of Surgery and Medical Education at the Recanati/Miller Transplantation Institute. Shirish S. Huprikar, MD, Associate Professor of Medicine and Director of Transplant Infectious Diseases at the Recanati/Miller Transplantation Institute, worked closely with the team to evaluate the appropriateness of HIV-positive donors.
Like Ms. Harry, all recipients must agree to participate in clinical research approved by each hospital’s Institutional Review Board under criteria set by the National Institutes of Health. It has been estimated that this new source of organs could be enough for as many as 2,500 additional deceased donor transplants in the United States each year.
New Appointments

Eric J. Nestler, MD, PhD, an internationally renowned neuroscientist and psychiatrist who has made significant contributions to our understanding of the molecular mechanisms of addiction and depression, has been appointed Dean for Academic and Scientific Affairs at the Icahn School of Medicine at Mount Sinai. Dr. Nestler is the Nash Family Professor of Neuroscience, and Director of The Friedman Brain Institute.
His research team explores the ways in which long-term exposure to stress or drugs of abuse change gene expression and chromatin structure within the brain’s reward circuitry, leading to addiction, or depression-like syndromes.
As Dean for Academic and Scientific Affairs, Dr. Nestler will oversee the Icahn School of Medicine’s basic research enterprise and all aspects of the Graduate School of Biomedical Sciences, and will provide a bridge for the educational programs of the Graduate School and the Department of Medical Education.
Dr. Nestler is a prolific writer and sought-after lecturer at scientific conferences. He is a member of the National Academy of Medicine and the American Academy of Arts and Sciences, holds many editorial posts, and serves as President-Elect of the Society for Neuroscience.

Joseph E. Herrera, DO, a noted clinician, educator, and researcher, has been appointed Chair and Lucy G. Moses Professor, Department of Rehabilitation Medicine, of the Mount Sinai Health System. He succeeds Kristjan T. Ragnarsson, MD, who led the Department for 30 years.
Dr. Herrera previously served as Chair of Physical Medicine and Rehabilitation at Mount Sinai Beth Israel, where he helped build highly selective residency and fellowship programs, and introduced innovative therapies, including the AposTherapy program, which uses specially designed shoes to alleviate chronic knee and back pain.
In his new role within the Mount Sinai Health System, Dr. Herrera will lead an effort to advance patient care through the use of new technologies, including robotics and phone apps. His clinical research interests include sports-related injuries, electro-diagnostic studies, fluoroscopic-guided spine and joint interventions, and the use of ultrasound for diagnosis and guided treatments.
Dr. Herrera treats amateur and professional athletes through an appointment to the New York State Athletic Commission and as Chief Team Physician for USA Boxing Metro.

Paul J. Kenny, PhD, the Ward-Coleman Chair in Pharmacology and Experimental Therapeutics, and an authority on the neurobiological mechanisms of addiction and obesity, now serves as Chair of the Department of Neuroscience. Dr. Kenny’s work has advanced the development of novel therapeutics that address those disorders.
His recent efforts in tobacco addiction have centered on a group of proteins known as nicotinic acetylcholine receptors (nAChRs) that consist of five subunits, each encoded by its own unique gene. (Previous research by a Mount Sinai scientist identified a mutation in one of those genes, CHRNA5.) Dr. Kenny’s lab played an important role in understanding how the CHRNA5 gene works. This opened a new window on nicotinic-receptor signaling in the brain and led to the finding that people who carry CHRNA5 variants are more likely to smoke, not because they enjoy nicotine more than others, but because they are resistant to adverse effects of the drug.
Dr. Kenny’s interests also include studying the role for novel regulatory RNA elements in brain cells —called microRNAs—in drug addiction and schizophrenia. Under his direction, Mount Sinai’s Experimental Therapeutics Institute is exploring the novel therapeutic potential of microRNAs.

René S. Kahn, MD, PhD, an authority on psychotic disorders, has assumed the role of Chair of the Department of Psychiatry. Dr. Kahn, the newly named Esther and Joseph Klingenstein Professor of Psychiatry, has dedicated his career to studying psychosis, particularly the origins and treatment of schizophrenia. His findings have informed clinical work in the field.
One of Dr. Kahn’s seminal discoveries was that schizophrenia starts in the early teenage years, earlier than previously thought, and that the first cognitive symptoms usually precede the first psychosis and visit to the psychiatrist by 10 years.
Using neuroimaging, Dr. Kahn has uncovered progressive changes in the brain over the course of schizophrenia that are linked to its severity. In his new role as Chair of Psychiatry, he plans to establish a specialized high-risk clinic to identify and treat individuals at an early age who are likely candidates for a range of psychiatric illnesses, as well as drug abuse.
The author of 800 research papers and book chapters, Dr. Kahn is also a member of the Royal Netherlands Academy of Science and a former Fulbright Scholar.