Mount Sinai Cardiologist Leads Effort to Outline Guidance for Management of Heart Failure Patients During COVID-19 Pandemic
New scientific statement aims to establish more streamlined care to improve outcomes in this high-risk group

A new scientific statement outlining unique considerations and suggestions for managing heart failure patients during the COVID-19 pandemic was issued today by the Heart Failure Society of America, and Anuradha Lala, MD, Assistant Professor of Medicine (Cardiology) at the Icahn School of Medicine at Mount Sinai, led the effort to advance this work. The document, published in the September 1 issue of Journal of Cardiac Failure, provides physicians with guidance on how to prevent heart failure and heart transplant patients from getting COVID-19 given their need for frequent monitoring; how to care for them if they get the virus; and the importance of vaccinations for both immunocompromised patients and those taking immunosuppressants.
This first-of-its-kind work is important to streamline care and protect this high-risk patient population. A previous Mount Sinai study conducted by Dr. Lala showed that heart failure patients hospitalized with COVID-19 are nearly twice as likely to die and at triple the risk of intubation when compared to those without the pre-existing heart disease.
“This document is the first of its kind to outline the issues unique to the nexus of heart failure and COVID-19. We believe this comprehensive document will be useful for internists and specialists alike, as well as patients and caregivers. Unfortunately, hospitals continue to face a surge of patients with COVID-19, including patients with heart failure, and/or history of mechanical circulatory support and heart transplant,” says Dr. Lala, the senior author. “Though much progress has been made in terms of our understanding of pathophysiology, development of vaccines, and processes of care, much work remains in understanding how the virus specifically exerts effects on the cardiovascular system and which treatments improve outcomes. Perhaps most importantly, this document underscores the need for our patients to be vaccinated and in some cases receive a booster vaccine.”
Dr. Lala and a team of international heart failure cardiologists, cardiothoracic surgeons, infectious disease physicians, pharmacists, and nurses developed this document based on accumulated data, peer-reviewed studies, and personal experience treating heart failure patients and heart transplant recipients throughout the COVID-19 pandemic. Their scientific statement outlines COVID-19’s impact on the heart and implications for clinical care. Several key points are highlighted:
- Telehealth for treatment and technology developed for remote monitoring of heart failure can help limit the risk of COVID-19 exposure for non-hospitalized patients, and physicians are increasingly relying on these tools.
- The authors provide a suggested algorithm for SARS-CoV2 testing of pre-transplant recipients and donors. For patients waiting for a heart transplant, COVID-19 testing should take place before transplant surgery, in addition to testing of the donor. Transplantation should be postponed if there’s a positive test, even if the patient does not have symptoms. This underscores the importance of mask wearing and social distancing and vaccination for patients on the transplant waiting list.
- Ideally and when feasible, health care workers caring for COVID-19 patients should avoid caring for hospitalized heart failure patients who are not COVID-19 positive.
- Heart failure patients and heart transplant recipients should be vaccinated, and patients who are immunosuppressed, including solid organ transplant recipients, should receive a third dose of mRNA COVID-19 vaccine, according to the Centers for Disease Control and Prevention (CDC)
- Despite initial fear that cardiac medications could lead to high risk of COVID-19, evidence has not supported this. Cardiac medications that are life-saving in the case of heart failure with reduced ejection fraction should be continued.
- Patients with heart failure should be considered eligible for all immunomodulating therapies (including monoclonal antibodies and steroids) used to treat COVID-19 patients, similar to populations without heart failure. Patients with heart failure may have more fluid overload when on these therapies so it’s important for physicians to look for and assess this, and then provide guidance on increasing diuretic medication.
- Vaccination rates remain lower than ideal for this vulnerable population. Designated efforts should be made to educate and inform patients of risks if they contract COVID-19 and to encourage vaccination as much as possible.
“This scientific statement rests on data accumulated to date but are subject to change as the field and research advances. Nonetheless, it is an important first step outlining unique considerations for this high risk population amidst this ongoing, virulent pandemic,” adds Dr. Lala.
Dr. Lala co-chaired the development of this scientific statement with Ankeet Bhatt, MD, a Clinical Research Fellow with the Division of Cardiovascular Medicine at Brigham and Women’s Hospital.
About the Mount Sinai Health System
Mount Sinai Health System is one of the largest academic medical systems in the New York metro area, with 48,000 employees working across seven hospitals, more than 400 outpatient practices, more than 600 research and clinical labs, a school of nursing, and a leading school of medicine and graduate education. Mount Sinai advances health for all people, everywhere, by taking on the most complex health care challenges of our time—discovering and applying new scientific learning and knowledge; developing safer, more effective treatments; educating the next generation of medical leaders and innovators; and supporting local communities by delivering high-quality care to all who need it.
Through the integration of its hospitals, labs, and schools, Mount Sinai offers comprehensive health care solutions from birth through geriatrics, leveraging innovative approaches such as artificial intelligence and informatics while keeping patients’ medical and emotional needs at the center of all treatment. The Health System includes approximately 9,000 primary and specialty care physicians and 10 free-standing joint-venture centers throughout the five boroughs of New York City, Westchester, Long Island, and Florida. Hospitals within the System are consistently ranked by Newsweek’s® “The World’s Best Smart Hospitals, Best in State Hospitals, World Best Hospitals and Best Specialty Hospitals” and by U.S. News & World Report's® “Best Hospitals” and “Best Children’s Hospitals.” The Mount Sinai Hospital is on the U.S. News & World Report® “Best Hospitals” Honor Roll for 2025-2026.
For more information, visit https://www.mountsinai.org or find Mount Sinai on Facebook, Instagram, LinkedIn, X, and YouTube.
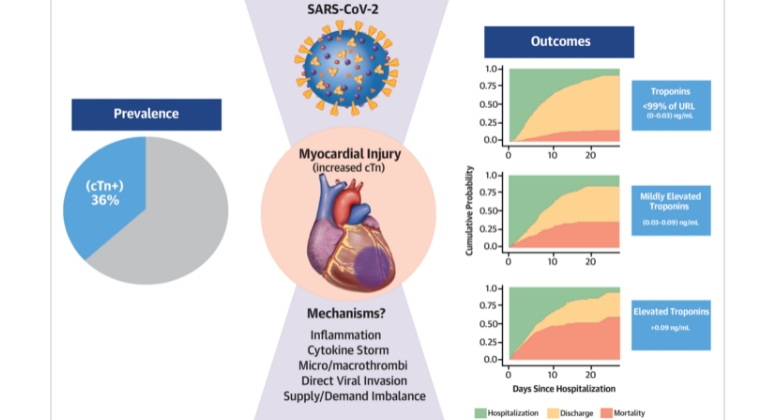
Heart Injury Among Hospitalized COVID-19 Patients Associated with Higher Risk of Death
Jun 08, 2020 View All Press Releases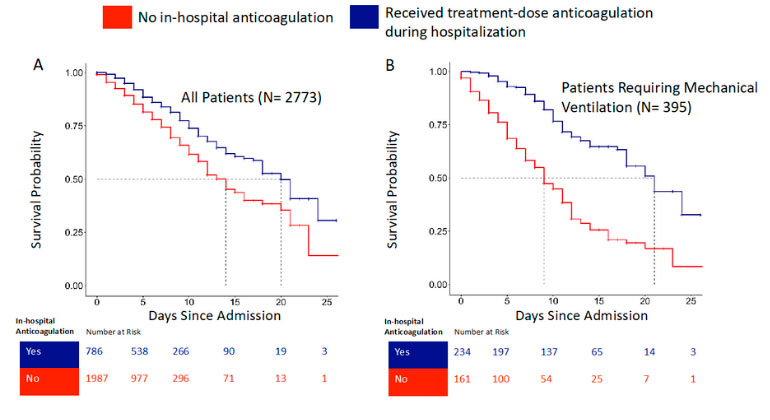
Blood Thinners may Improve Survival among Hospitalized COVID-19 Patients
May 06, 2020 View All Press Releases