PCORI Approves $54.8 Million For Clinical Effectiveness Research
The Patient-Centered Outcomes Research Institute approved $54.8 million for 33 clinical effectiveness projects.
The projects, approved by the institute's board of governors July 29, will study ways to improve outcomes for patients with cancer and other diseases, including diabetes, nervous system disorders, cardiovascular diseases, mental health conditions and kidney diseases. The studies will compare different approaches to delivering care, improving patient access, and patient-centered clinical effectiveness research methods. Several projects will focus on particular populations, including older adults, minorities, children and low-income individuals.
Selected from 325 applications from funding announcements issued in September 2013, the approved studies are based at institutions and organizations across 18 states. All awards were approved after a business programmatic review by PCORI staff and issuance of a formal award contract, the institute said. PCORI is refining their funding announcements to focus on priority topics and larger, pragmatic studies, said the institute's executive director, Joe Selby. Since it began funding research in 2012, PCORI has approved nearly $549 million in support of 313 research projects and initiatives. The institute said it expects to award about $1 billion in research support by the end of next year.
Nina Bickell, Professor of Medicine from the Population Health Science and Policy at Mount Sinai School of Medicine, proposed a three-year, $2 million project to study and improve patient care for late-stage cancer. "Among advanced cancer patients, discussions about prognosis, goals of care, and end-of-life preferences improve patients' quality of life and reduce hospital and ICU admission rates," the project summary states. "Yet, few patients know their chemotherapy treatments will not cure their disease, despite nearly all wishing to receive both positive and negative information."
Dr. Bickell's project seeks to improve goals-of-care discussions by training oncologists to better communicate and understand the effects their discussions have on the patients. "Current efforts to teach oncologists such skills are impractical; they require a lot of time away from the physicians' office practice and do not take into account job pressures," the summary says. "Primary outcomes include patient-reported conduct of and satisfaction with the [goals-of-care] discussion. Secondary outcomes include oncologist communication skills; feasibility of performing [goals of care] in the outpatient setting; receipt of care in line with preferences; and use of hospice, chemotherapy, or ICU in the last 30 days of life."

“Forever Chemicals” Linked to Higher Risk of Type 2 Diabetes
Jul 22, 2025 View All Press Releases
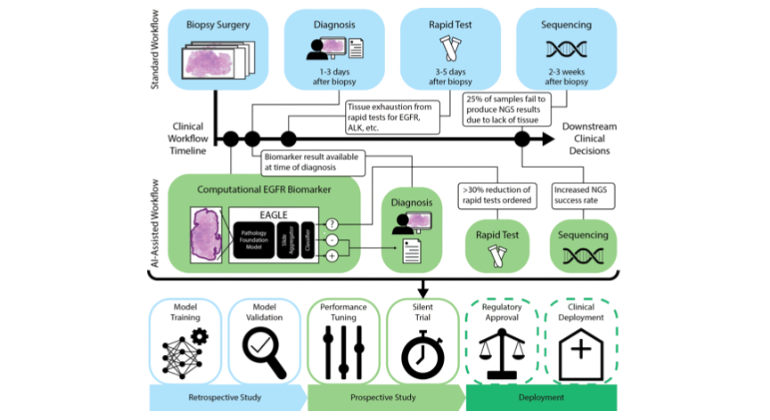
Like Humans, AI Can Jump to Conclusions, Mount Sinai Study Finds
Jul 22, 2025 View All Press Releases
Mount Sinai Researchers Engineer Rare Immune Cells to Create Powerful New Cancer Vaccine
Jul 21, 2025 View All Press Releases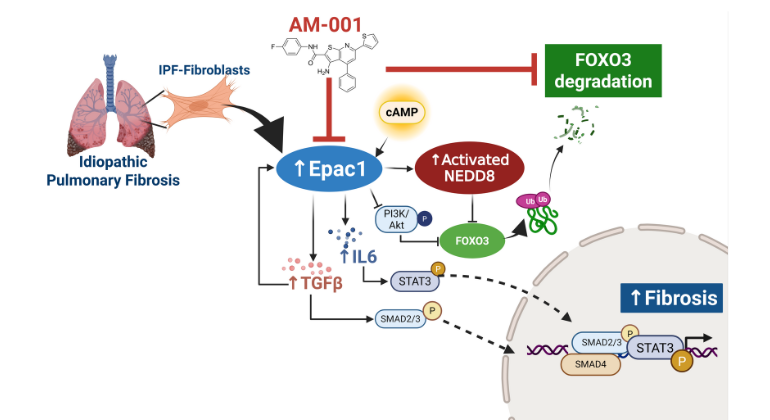
Blocking a Little-Known Protein May Offer New Hope for Devastating Lung Disease
Jul 15, 2025 View All Press Releases
Prenatal and Childhood Lead Exposure Linked to Faster Memory Decay in Children
Jul 09, 2025 View All Press Releases
The New England Journal of Medicine Shines Spotlight on Forensic Pathology
Jul 03, 2025 View All Press Releases