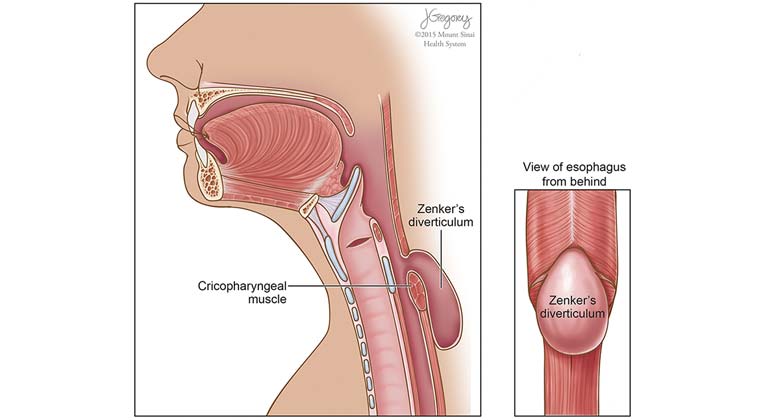
Zenker’s Diverticulum
A Zenker’s diverticulum is an outpouching that occurs at the junction of the lower part of the throat and the upper portion of the esophagus. The pouch forms because the muscle that divides the throat from the esophagus, the cricopharyngeal (CP) muscle, fails to relax during swallowing. The arrangement of muscles in the lower part of the throat, medically known as the hypopharynx, helps support and elevate the pharynx during swallowing. To be efficient in this function, these throat muscles, medically called the constrictors, are arranged at an angle. When we swallow, the brain signals the throat muscles in the hypopharynx to contract. In contracting the muscles of the hypopharynx, the constrictors, elevate the larynx and throat and push the food into the esophagus.
The top of the esophagus is defined by the CP muscle that surrounds the top of the esophagus in a horizontal fashion. The CP muscle is chronically under tension. It functions to keep food in the esophagus between swallows. When we swallow, milliseconds after the throat or pharyngeal muscles contract, the brain sends a signal to the CP muscle to relax and allow the food to go from the throat into the esophagus.
Because the pharyngeal muscles, the constrictors, are at an angle, and the muscle at the top of esophagus, the CP muscle, is horizontal, there is a week area of the pharynx that often does not have muscle. This is a triangular space and is called Killian’s triangle. The size of this space is genetically determined. If the CP muscle at the top of the esophagus does not relax completely or quickly enough, the food that is being swallowed is pushed against the top of the esophagus at the CP muscle and the weak area in Killian’s triangle is pushed out. Eventually a pouch, a Zenker’s diverticulum, can form.
At The Grabscheid Voice and Swallowing Center, our interdisciplinary team of speech language pathologists and laryngologists are experienced in evaluation and management of patients with Zenker’s diverticulum. During your consultation, you will undergo complete swallow evaluation to determine which types of interventions will best help relieve your symptoms. Our speech language pathologists are adept in performing evaluations of swallowing and helping patients rehabilitate their swallowing without surgery if that is in the patient’s best interest. Our surgeons are also versed in the evaluation of swallowing and are highly experienced in all types of surgery for relief of symptoms in patients with Zenker’s diverticulum.
Symptoms of Zenker’s Diverticulum
Patients with a Zenker’s diverticulum experience symptoms when food or secretions get stuck in the pouch. These are usually first noted during the 5th to 7th decade of life. Because the bottom of the pouch is lower than the opening into the throat, secretions and food particles build up in the pouch. Patients feel a need to clear their throat periodically throughout the day or 20 or so minutes after a meal. The solid food particles lodge in the pouch and at times the patient needs to regurgitate these or manually empty them. This causes patients to subconsciously alter their diet to softer foods that are easier to eat and not as difficult to empty from the pouch. If meals are too unpleasant, patients can begin to eat less and then lose weight.
Often the pouch fills and then empties spontaneously into the bottom of the throat causing the patient to cough. Patients with symptoms of Zenker’s for a long time have an increase risk and incidence of pneumonia from aspirating these contents. Finally, some patients complain of a belching noise that occurs with swallowing as air trapped in the pouch is squeezed out s the patient is compressed during swallowing.
Zenker’s Diverticulum Evaluation
Patients with difficulty swallowing should have a thorough evaluation beginning with a history specifically attempting to identify the symptoms described above. These symptoms are considered diagnostic. After a history, the patient should undergo examination of the pharynx (throat) and larynx (voice box). This examination can be accomplished with either a flexible telescope through the nose (flexible endoscopy) or a rigid telescope or mirror (indirect laryngoscopy) through the mouth. The purpose of this exam is to identify patterns of pooling of secretions in the throat and to examine the strength of the tongue and throat muscles.
Since Zenker’s occur in older people and because older people have weaker throat muscles and more difficulty with swallowing in general, it is critical that the physician examine the throat for overall function and health. Isolated pooling of secretions in the left side of the throat is highly associated with Zenker’s diverticulum. If the remainder of the pharynx is healthy and does not collect secretions, then it is likely that patients will do well with surgical elimination of the diverticulum. However, if the entire pharynx is weak, then even if the Zenker’s diverticulum is removed, the patient may still have difficulty swallowing. Therefore, patients should also undergo a radiographic assessment of swallowing that is video-taped preferably at greater than 30 frames per second. This type of recording, called a modified barium swallow (MBS) will allow the surgeon to review and assess the entire swallow mechanism accurately and in detail. If the exam is recorded at less than 30 frames per second important details of the act of swallowing could be missed. This can result in performance of surgery that is not helpful because details of swallowing deficits are not identified.
Treatment of Zenker’s Diverticulum
Once the Zenker’s diverticulum is identified and it is determined that it is the cause of the swallowing difficulty, then treatment options can be considered. Surgery is the standard of treatment but, for older or infirmed patients, life style and dietary modifications can be considered.
Dietary Modifications
Since most symptoms occur due to retained solid foods, patients can choose to adopt a pureed or full-liquid diet. By working with a dietician, meals can be made to be enjoyable and to provide enough caloric intake to maintain weight and a good quality of life. Patients who choose this option will likely still cough on retained secretions and be at increased risk of aspiration and pneumonia. Therefore, they must be instructed on oral hygiene measures. They need to eat slowly so that food does not build up in the diverticulum. The patient should also be instructed to reduce the bacterial count in their mouth by brushing their teeth before and after every meal. In this manner if or when food is aspirated, it will be less likely to bring harmful bacteria into the lungs.
Surgical Management of Zenker’s Diverticulum
Patients with preserved pharyngeal strength and swallow reflexes are excellent candidates for surgical correction. Since the main reason the diverticulum forms is failure of relaxation of the CP muscle, surgeons have found that surgical intervention is most effective when it targets cutting the CP muscle. Historically surgeons attempted to suspend the diverticulum or cut it out, but did not address the CP muscle. These procedures led to a high rate of recurrent symptoms. Subsequently surgeons began cutting the CP muscle. Originally CP myotomy was performed through and incision in the neck. While this is still a viable option and is associated with highest long-term success rate of surgery, , especially for patients with larger diverticulum, it is associated with a higher rate of complications such as vocal fold nerve paralysis, infection and esophageal perforation as well as a prolonged postoperative healing phase.
For patients requiring surgery, minimally invasive surgery is now the preferred first line approach. In this surgery, the CP muscle is cut by approaching it through the mouth. When performed carefully by a surgeon experienced in minimally invasive approaches, the surgery has at least an 85% long-term success rate for relief of symptoms. These minimally invasive approaches can be successful for patients with small and large diverticulum provided the surgeon understands the nuances involved with modifications for large and small diverticulum. With minimally invasive approaches, an incision in the neck is not needed, the vocal fold nerves are not placed at risk and patients can usually be home and a soft diet after only one night in the hospital. In addition, if the patient is in the 15% who have recurrent symptoms, the minimally invasive approach can often be revised or an open approach can be undertaken.