Pediatric Craniofacial Program (Cranial Disorders and Head Shape)

Craniofacial conditions affect the growth and development of a child’s skull, face and brain. These conditions are often present at birth (congenital) and can typically be diagnosed in infancy. A newborn's skull is made up of bony plates separated by flexible spaces called sutures, which allow the skull to grow with the brain. During regular checkups, your pediatrician will monitor your baby’s head shape, growth, and developmental milestones. When abnormalities are identified, early referral is key.
Our Craniofacial Program at Mount Sinai provides specialized, family-centered care for infants and children with head shape and facial differences. Our expert team—including pediatric neurosurgeons, plastic surgeons, neurologists, geneticists and others—works collaboratively to diagnose and treat a wide range of craniofacial conditions. We offer both minimally invasive and traditional surgical options, always tailored to your child’s unique needs. From diagnosis through treatment and long-term follow-up, we are here to support your child’s health, development, and confidence—every step of the way.
Common Conditions We Treat
Craniofacial conditions may be noticeable at birth or become more apparent over time. Subtle differences in head shape or facial features can indicate:
- Craniosynostosis – Premature closure of one or more skull sutures, affecting head shape and brain development
- Plagiocephaly – Flattening of one part of the head, often caused by external pressure
- Cleft Lip and Palate – Openings in the lip and/or roof of the mouth that occur during fetal development
- Hemifacial Microsomia – Underdevelopment of one side of the face
- Pierre Robin Sequence – A small lower jaw, tongue displacement, and breathing difficulties
- Apert, Crouzon, and Pfeiffer Syndromes – Genetic conditions that impact skull and facial growth
Early diagnosis and evaluation help prevent complications and support your child’s developmental progress.
Signs and Symptoms
If your child has a craniofacial condition, you may notice:
- Abnormal head shape or facial asymmetry
- Visible ridges along the skull
- Uneven features or skull flattening
- Breathing, feeding, or vision issues
- Developmental delays or signs of increased intracranial pressure like headache or blurry vision
Evaluation and Diagnosis
If there are concerns about your child’s head shape, our team will perform a thorough clinical evaluation. This may include:
- A detailed physical examination
- Imaging (such as CT scans)
- Ongoing monitoring to assess skull growth over time
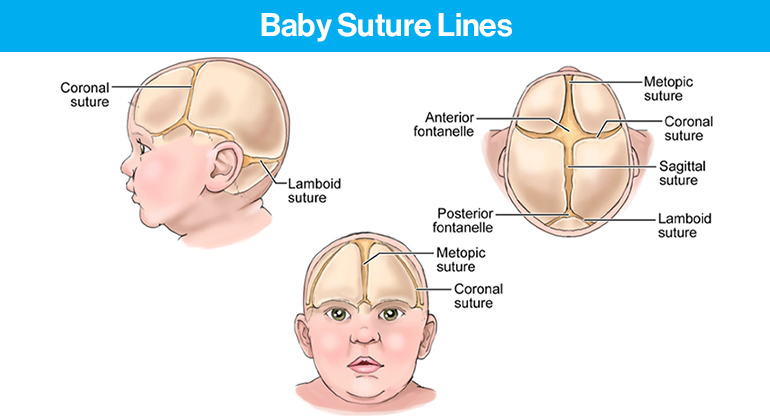
Understanding Skull Sutures
The skull consists of several sutures that typically close at different ages:
- Metopic Suture – Forehead to nose; usually closes by 12 months
- Coronal Sutures – From the top of the head to each ear; close around age 2
- Sagittal Suture – Midline on top of the head; closes around age 2
- Lambdoid Sutures – Back of the head; close after age 2
Craniosynostosis occurs when one or more of these sutures close too early, which may require surgical correction to allow for normal brain growth.
What to Do If You’re Concerned
If you notice any abnormalities in your child’s head shape—or if your pediatrician recommends further evaluation—please reach out to our team:
- Call: 212-241-0954
OR - Email: pedsneuro@mountsinai.org
We will schedule a consultation, review your child’s history, conduct an evaluation, and determine whether imaging or treatment is necessary. Many children require only monitoring, while others may benefit from a multidisciplinary approach.
If Your Child Is Diagnosed
If your child is diagnosed with a craniofacial disorder, our team will guide you through every step of care. If surgery is needed, we will explain all options—from minimally invasive techniques to open cranial vault remodeling—and provide compassionate support before, during, and after the procedure.
Together, we’ll create a personalized care plan that puts your child’s health, comfort, and development first.
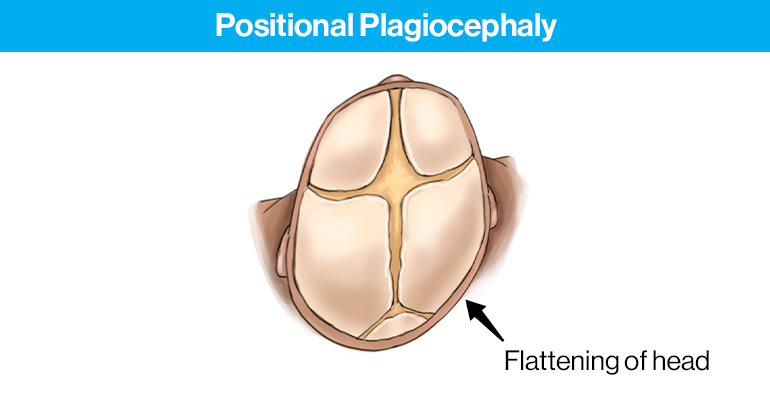
Positional Plagiocephaly
In response to evidence that sleeping on the back reduces the risk of SIDS (Sudden Infant Death Syndrome), babies are put on their backs to sleep. The recommended “Back to Sleep” campaign, though the safest position, commonly results in increasing frequency of positional plagiocephaly, or the flattening of the back of the head. Your baby’s flat head can be symmetrical or favor one side and sometimes can be worsened by a condition called torticollis, where the neck muscles on one side are too stiff.
In positional plagiocephaly, flattening of the back of the head is often accompanied by changes in the shape of other parts of the head to compensate and allow brain growth. These can include anterior displacement of the ear and slight prominence of the forehead on the same side affected by the flattening.
Usually, the head flattening and compensatory changes improve on their own as the child becomes more mobile. As this is a cosmetic concern and should not affect brain development, repositioning, physical therapy and occasionally a helmet may be used, when appropriate.
Diagnosing Plagiocephaly
Seeing the difference between plagiocephaly and craniosynostosis requires a clinically trained eye. Though plagiocephaly is much more common, a missed diagnosis of is craniosynostosis can lead to delayed treatment and worsening of your child’s condition.
Evidence-based guidelines recommend that even in moderate to severe cases of positional plagiocephaly, helmets may be considered if observation, repositioning therapy and physical therapy are unsuccessful.
Plagiocephaly Treatment Options
Repositioning, Tummy Time, and Therapy
Conservative management is first line therapy and includes emphasis on mindful repositioning and encouragement of tummy time while the child is awake. Physical therapy can also be used as supplementation for any motor conditions that contribute to worsening the flattening, such as torticollis, a side preference, or weakness. These exercises usually help strengthen these deficits reducing time spent on the back of the head, leading to improvement of head shape.
If your child does not respond to conservative treatment, has severe motor deficits, or is diagnosed at a later age, then helmet therapy may be considered.
Helmet Therapy
Helmet therapy, or cranial orthosis, has been used widely to:
- Improve head shape in positional plagiocephaly
- Guide growth of the skull after minimally invasive craniosynostosis repair
If it is determined that your child would benefit from a helmet our team will provide you with a referral. Children are recommended to wear these helmets for 23 hours per day, for a variable period of time. Most children wearing helmets will have regular follow-up visits with the orthotist to track progress and determine when helmet therapy is complete. It is important to continuously monitor for skin damage when helmets are used.
Craniosynostosis
In craniosynostosis there is a premature fusion of one or more cranial sutures, resulting in restricted growth of the skull in ways that are unique to each suture. The appearance of the head shape will differ depending on which sutures are fused.
Craniosynostosis is a condition treated with surgery, as there are no medicines or non-surgical measures that are effective at correcting the problem. Our experienced craniofacial team consists of experts in the diagnosis and treatment of craniosynostosis involving all sutures and will take you through the steps of pre-surgical evaluation, surgical treatment options, and after-care. We will answer all your questions and prepare you, your child, and your family for the treatment plan with the best outcome.
Diagnosing Craniosynostosis
Craniosynostosis can be detected as early as birth. It is important to diagnose craniosynostosis in a timely manner to facilitate normal skull and brain development, as well as allow for the option of a minimally invasive surgical approach.
It can at times be difficult to differentiate normal physiologic development from craniosynostosis. A formal diagnosis can usually be made with a physical examination, but sometimes more subtle findings may require imaging. An ultrasound evaluation of the suture lines can assist in diagnosis and does not emit radiation. Sometimes an x-ray or CT scan is necessary for more definitive evaluation of the suture lines or for surgical planning purposes. If a CT scan is required, Mount Sinai’s pediatric CT scanning protocol will minimize the radiation dose for your child.
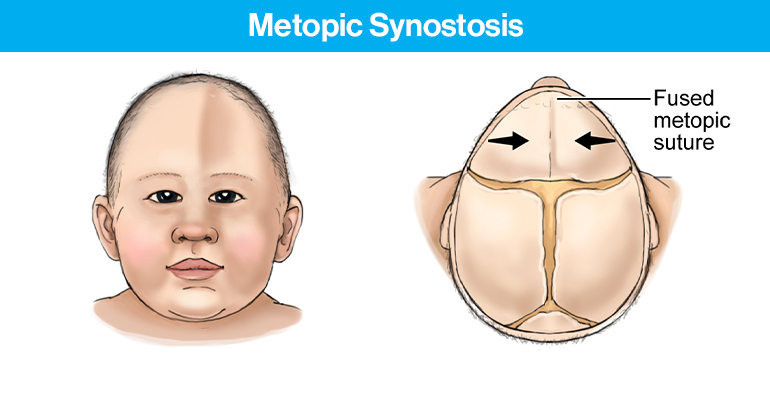
Metopic Synostosis
Your child will have a narrow, triangular-shaped forehead head, often with a midline forehead ridge, and eyes appearing close together. There is also often widening of the back of the head.
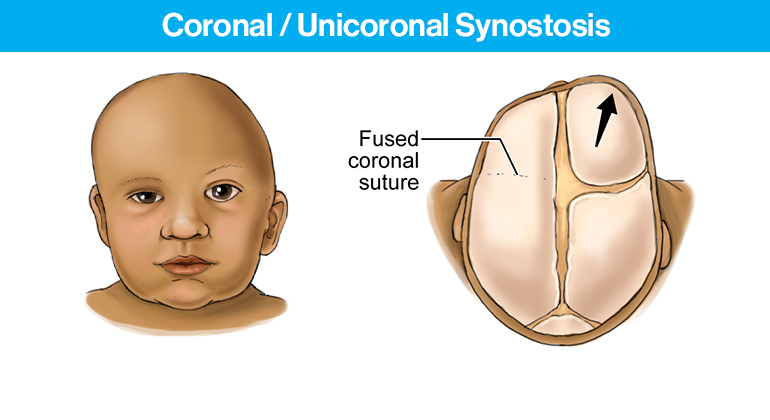
 Coronal/Unicoronal Synostosis
Coronal/Unicoronal Synostosis
Your child’s forehead and brow will be flattened, and one eye may be shaped differently on the affected side. Forehead prominence is present on the opposite side. When bilateral craniosynostosis occurs, the entire forehead tends to be tall and flat.
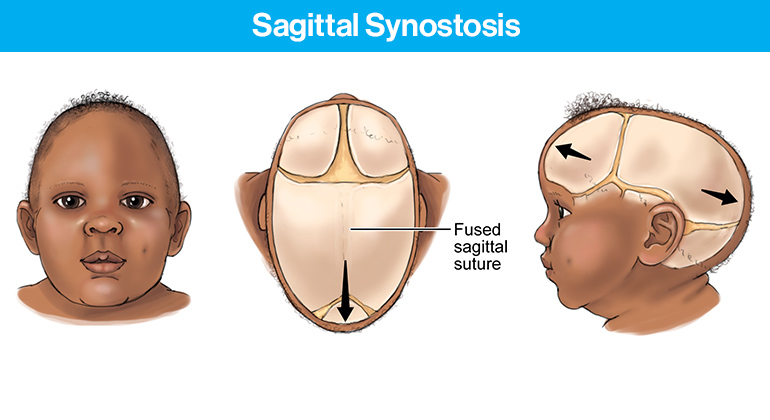
 Sagittal Synostosis
Sagittal Synostosis
Your child will have a long, narrow appearance of the head when viewed from above. There can also be fullness (bossing) and increased height of the forehead or back of head.
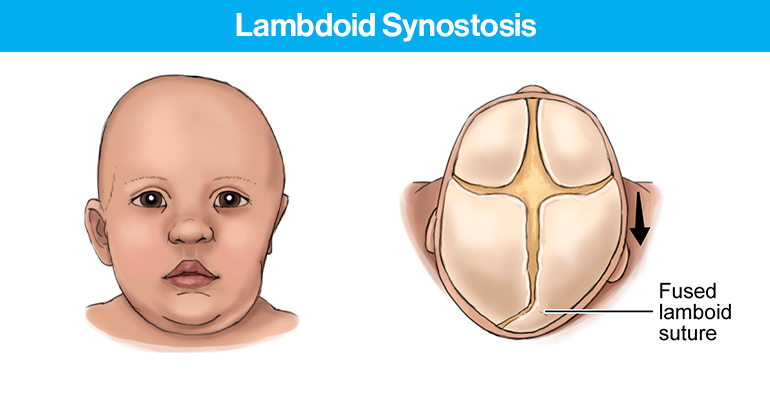
 Lambdoid Synostosis
Lambdoid Synostosis
One side of the back of your child’s head may appear flat. The ear on the affected side is pulled back and there is often a bulge of bone below and behind the ear.
Craniosynostosis Treatment Options
Surgical planning is carefully considered and developed on a case-by-case basis by our pediatric neurosurgeons and craniofacial plastic surgeons. As a team, we discuss appropriate surgical options for your child.
Our goal is to provide a true understanding of your child’s unique condition, how we will perform the surgery, immediate and future recovery expectations, and what to monitor at home. We assure you that we’ll always be available to answer all of your questions and design the best plan for your baby.
Endoscopic Surgery
Our pediatric neurosurgeons at Mount Sinai offer minimally invasive endoscopic surgical procedures to infants who are younger than three months of age (and in select cases in older babies) with craniosynostosis.
- Surgical Approach
This surgical approach involves making a 2-3cm incision over the affected suture. Using an endoscope for visualization, a strip of bone is removed at the fusion point creating free movement of the cranial plates at that location in your child’s skull. - Recovery
The hospital stay post-operatively is about one to two days. Typically, after surgery, your child’s head may appear puffy or swollen at the surgical site. We will have a post-operative visit two weeks after surgery to evaluate your child’s progress and to check the incision site. After the incision has healed, a helmet is typically used to guide the growth of the skull for a period of several months to a year. Helmets are worn throughout the day and night, only removed for bathing, and they require frequent evaluations and adjustments by the helmet clinic.
Open Cranial Reconstruction
In babies older than three months with craniosynostosis, our pediatric neurosurgeons and pediatric plastic surgeons work together to perform a surgical repair known as “cranial vault remodeling.” This allows the neurosurgeon and craniofacial plastic surgeon to correct the head shape and any associated upper facial abnormalities simultaneously.
- Surgical Approach
Craniosynostosis surgery usually lasts three to four hours and involves reshaping the skull bones to achieve a normal head shape. The precise type of reconstruction varies based on the type of craniosynostosis and your child’s individual anatomy. - Recovery
Children who undergo cranial vault remodeling typically spend three to five days in the hospital PICU after surgery and return home as the swelling of the scalp and eyelids diminishes.
These children do not require helmet therapy to correct the head shape, as the entire correction is completed during the surgery.
Meet Our Team
There is not just one person dedicated to the care of your child. We work as a team with pediatric neurosurgeons, craniofacial plastic surgeons, and neurologists. For cases that require more involved specialty care, our team has geneticists, specialized pediatricians, specialized rehabilitation physicians and physical therapists, and pediatric ENTs. As a team, we discuss all options for your child.
Saadi Ghatan, MD
Pediatric Neurosurgeon
Peter F. Morgenstern, MD
Pediatric Neurosurgeon
Meg Pain, MD
Pediatric Neurosurgeon
Peter J. Taub, MD
Pediatric Craniofacial Plastic Surgeon