Using the Senses to Identify Stroke
Mount Sinai Neurologist Carolyn Brockington, MD, discusses the warning signs offered by vision, hearing, and other senses

Congratulations, Dr. Helen Mayberg
Leading Mount Sinai Brain Scientist Elected to the National Academy of Sciences
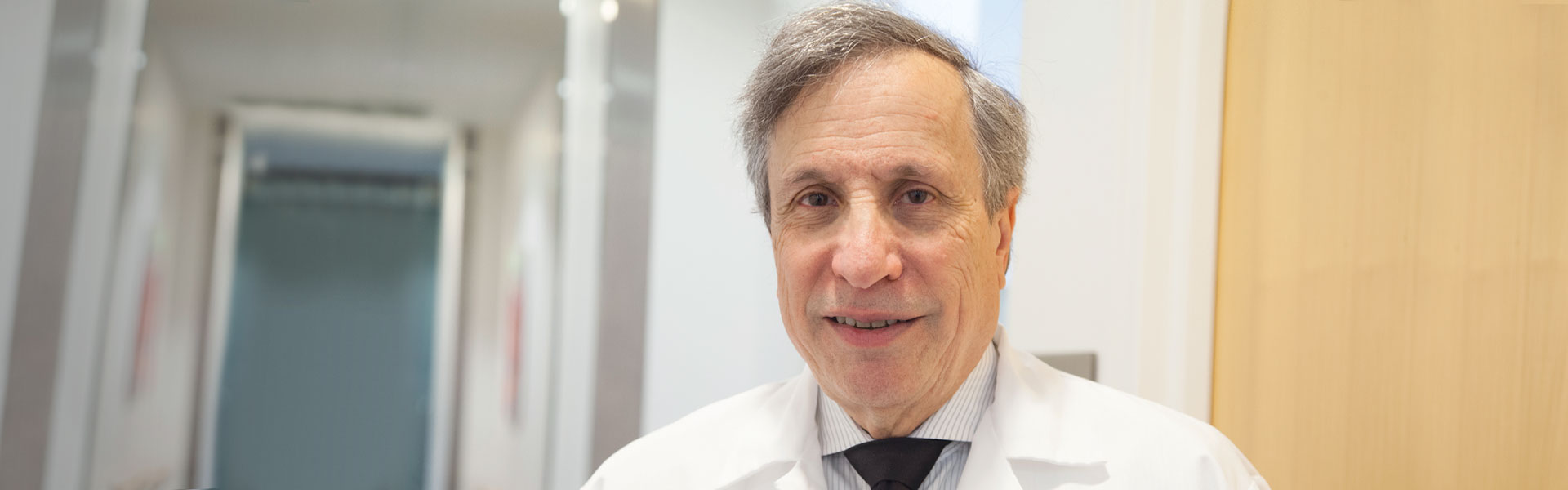
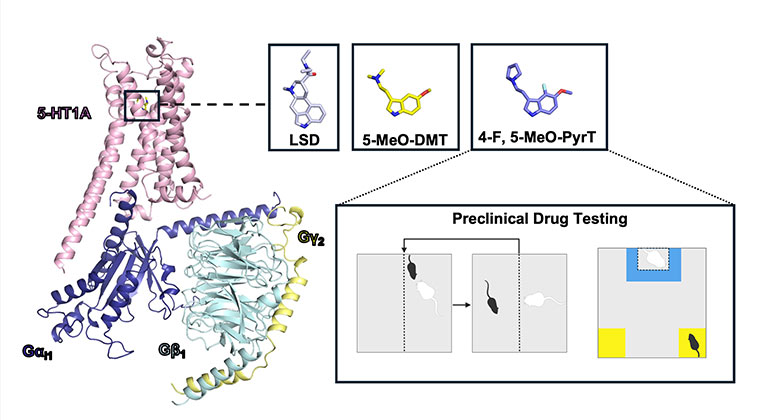
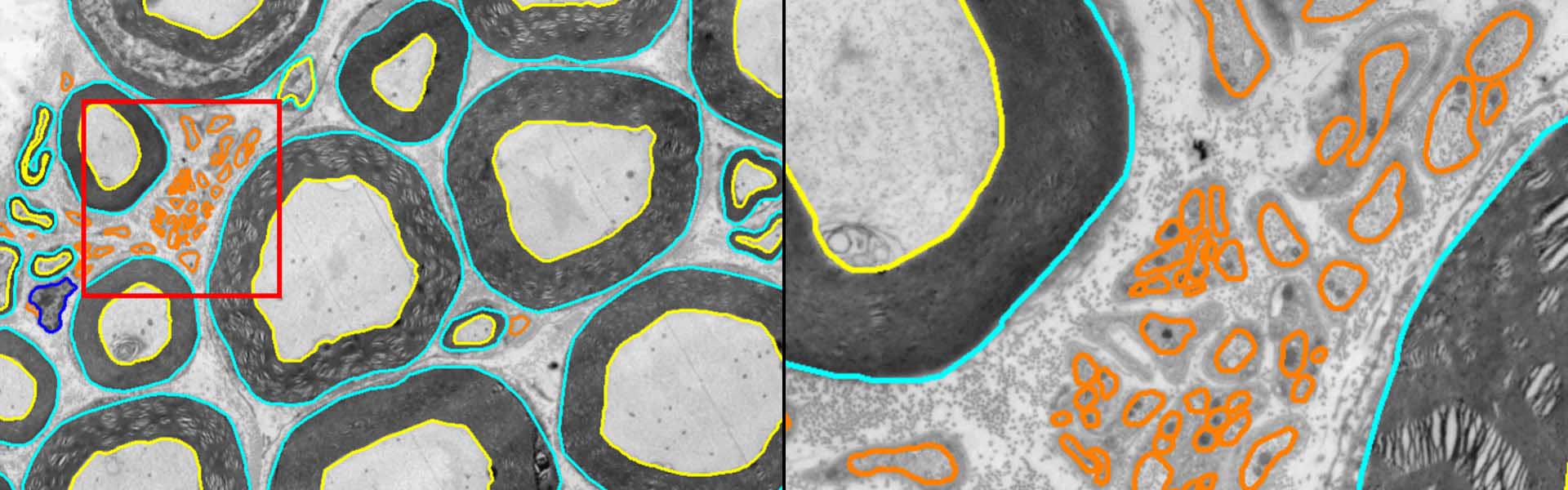
New Research on MS and Disability
Fred Lublin, MD, Director of the Corinne Goldsmith Dickinson Center for Multiple Sclerosis, is lead author on a new study on how patients with MS acquire disability.
Infant’s Rare Spinal Defect Is Detected and Repaired by Mount Sinai Doctors
Thanks to early diagnosis and a successful surgery, Philip celebrated his first birthday a month after discharge.
Neurology Telemedicine Appointments
We are proud to offer virtual care appointments for certain visit types with our neurologists.
Neurology Specialty Report
We are dedicated to rapid advances in technology, pioneering research, and multidisciplinary collaboration to set a new standard for team care to dramatically improve the quality of life for patients

Compassionate Care
Providing Patients with Movement Disorders Treatment Tailored To Their Needs

A Multidisciplinary Approach
Improving Quality of Life for People Living with Multiple Sclerosis
Neurology
Neurology
When it comes to finding care for a neurological condition, you want the best medicine, backed by the newest research, and delivered by highly skilled doctors who take the time to develop a relationship with you and your family. We believe every patient who walks through our door deserves exactly that combination of science and personalized attention – whether you are an inpatient seen by one of our neurohospitalists or are seeking outpatient care at one of our many locations.
Our approach starts simply: We listen to you. After hearing about your symptoms and answering your questions, we’ll guide you through the most advanced testing to make a thorough and accurate diagnosis. From there, we offer the newest treatment options, informed by innovative research conducted right here at the Icahn School of Medicine at Mount Sinai. Our physicians specialize in the full range of neurological conditions in children, adolescents, and adults – including stroke, epilepsy, headache, Parkinson’s disease, multiple sclerosis, brain and spinal tumors, Alzheimer’s disease, and amyotrophic lateral sclerosis (ALS) – and work with a trained team of nurses, social workers, neuropsychologists and others to customize the right treatment plan for you and your family.
The Mount Sinai Hospital is ranked among the top 20 in the nation for Neurology and Neurosurgery by U.S. News & World Report® for 2024-25. We are committed to combining our scientific expertise with the compassionate, individualized attention you need to enjoy the best possible health.
Neurological Care at Mount Sinai Health System


Cognition and Behavior
Our cognitive and behavioral specialists provide interdisciplinary care for people with cognitive and behavioral concerns, including Alzheimer's & other dementias
Learn More
Epilepsy Center
Providing expert care for children and adults with epilepsy and related disorders
Learn More
General Neurology
Our neurologists have extensive experience in diagnosing and managing neurological disorders
Learn More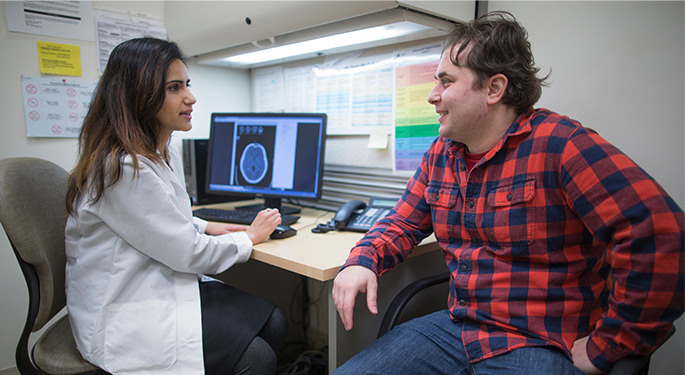
Headache and Facial Pain
Diagnosis and treatment of acute and chronic headaches and facial pain
Learn More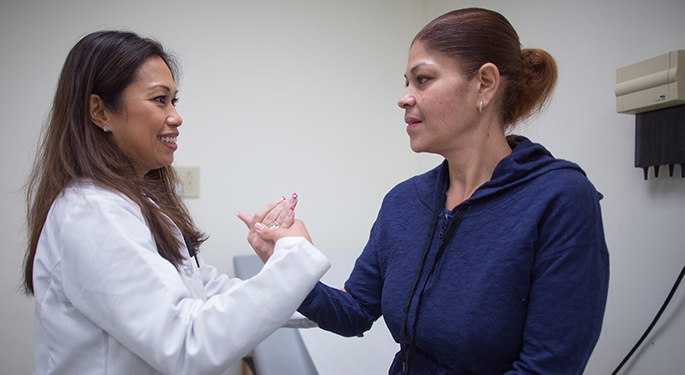
Movement Disorders
Providing expert diagnosis and management of Parkinson’s disease and other movement disorders in adults and children
Learn More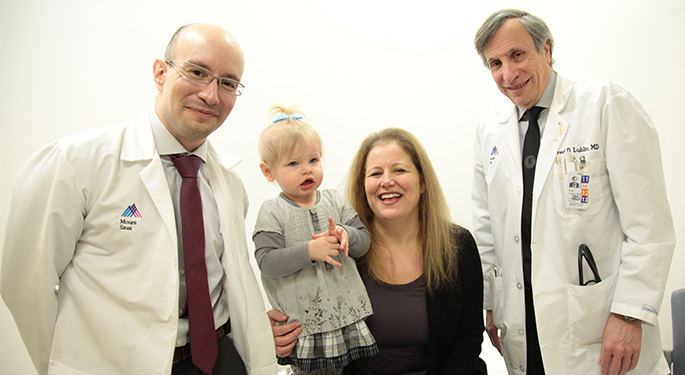
Multiple Sclerosis and Neuroinflammatory Disorders
Diagnosing and treating multiple sclerosis and related disorders
Learn More
Neurofibromatosis
The NF clinic at The Mount Sinai Hospital serves as a one-stop medical “home” for NF patients, who often need to coordinate care with multiple experts.
Learn More
Neurogenetics
A division dedicated to the diagnosis and treatment of patients with neurological manifestations from rare genetic diseases.
Learn More
Neuromuscular Disease
Diseases that affect the peripheral nervous system are treated here
Learn More
Neuro-Infectious Diseases
Treating the neurological infections that impact areas of the brain
Learn More
Neuro-Oncology
Offering a comprehensive approach to the treatment of patients with brain tumors, spinal cord tumors, and more
Learn More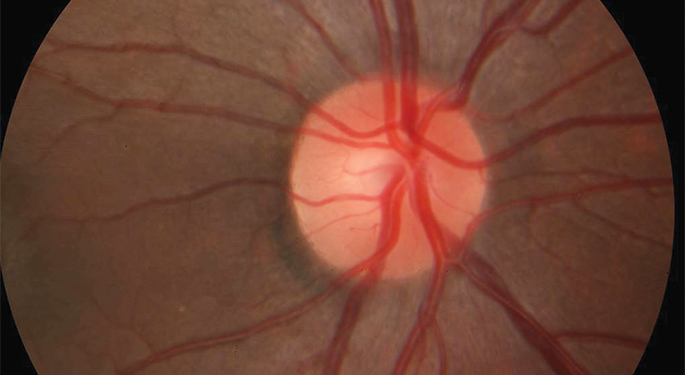
Neuro-Ophthalmology
Specializing in evaluating, diagnosing, and treating visual problems related to the nervous system
Learn More
Neuro-Otology
Providing cutting-edge treatment for patients with balance problems and dizziness
Learn More
Pediatric Neurology
Combining compassionate care with expertise to provide the best in pediatric neurology
Learn More
Stroke / Cerebrovascular Disorders
Offering state-of-the-art care to stroke patients and their families
Learn More