After a Heart Attack and 5 Months in the ICU, Brooklyn Grandfather Receives a Life-Saving Heart Transplant
On September 8, 2022, Carlos Toro started to experience some chest pain while he was at work at his supermarket job. It didn’t seem like much to worry about, and he spent the next day in his backyard doing carpentry work for local children’s playgrounds, as he often did in his spare time. However, by the following night his symptoms had returned, with a strong pain starting in his abdomen that spread to the left of his chest cavity.
He drove himself to the Emergency Department at Mount Sinai Brooklyn, eight minutes away. There, the team carried out an EKG and discovered he was suffering from a severe heart attack. The next day he was transferred to Mount Sinai Beth Israel in Manhattan.
“I go every year and have my physical and have my checks,” Carlos says. “And I was never put on any kind of medication except for a hypertension prescription at a very low dosage. I was astonished when they told me that I was having a massive heart attack. And then everything changed after that.”
Within hours of his arrival at Mount Sinai Beth Israel, Ramesh Gowda, MD, Co-Director of Cardiac Cath Lab, and a specialist in interventional cardiology and endovascular medicine, carried out a left heart catheterization. This is a procedure where a thin flexible tube (catheter) is inserted into the left side of the heart to check for blockages in the arteries. Dr. Gowda and his team discovered that the left main artery was completely blocked and inserted stents to open up the artery.
After the procedure, a balloon pump was placed to help support Carlos’ heart. When the pump was removed after 48 hours, his heart function began to decline again. The team then performed a right heart catheterization. This procedure provides information regarding hemodynamics (blood flow) and monitors the level of pressure in and around the heart to help guide the patient’s treatment. The test revealed that his heart wasn’t pumping effectively and fluid was accumulating in his lungs. An ultrasound of his heart confirmed he had a significantly reduced ejection fraction (the rate at which blood is being pumped out with each heartbeat). A normal ejection fraction is above 55 percent—Carlos’ ejection fraction was 29 percent.
A diagnosis of heart failure
He was diagnosed with heart failure and was transferred to the Intensive Care Unit (ICU) at The Mount Sinai Hospital, where he was put on guideline-directed medical therapy—a set of four drugs used to manage heart failure. After a week, his condition had stabilized enough for him to return home.
However, during the next few weeks, Carlos started to suffer from intense pain at night, and he was not able to sleep due to increasing shortness of breath. At the end of October, he had an episode of breathlessness that was severe enough for him to call 911. He was readmitted to hospital with heart failure exacerbation (a worsening of heart failure symptoms).
Dr. Gowda referred him to Johanna Contreras, MD, Associate Professor of Medicine (Cardiology) at Icahn Mount Sinai and a specialist in heart failure and heart transplantation. She initiated a heart failure workup, and the tests revealed significant scarring of the heart muscle. “When the heart muscle doesn’t get enough blood, eventually that muscle will die and scar tissue will form, and even if you give blood to it, it won’t come back to life,” Dr. Contreras explains.
“We have to try and get you a heart”
Another readmission in December 2022 and a visit to the Emergency Department in January 2023 indicated that the guideline-directed medical therapy was not going to be a long-term solution for Carlos. In February 2023, Dr. Contreras explained to him that he was running out of options and that he needed to consider having a heart transplant. “His blood pressure was so low that he couldn’t really tolerate any more medications. I told him we need to consider a heart transplant,” Dr. Contreras says.
Initially, Carlos was unsure about whether he wanted to go ahead with a heart transplant. “I told Dr. Contreras that I appreciated everything that she was doing for me, but maybe it was my time. And she said, ‘No, Carlos, you're too young! We have to try and get you a heart.’ I feel like she saved my life by saying that. From there on, I just did whatever she told me. I knew that she was rooting for me.”
Dr. Contreras started the assessment process for a heart transplant, including a visit with a psychiatrist and screenings for cancer and other conditions. Carlos was found to be a good fit for a transplant, and in April 2023, he met with Anelechi Anyanwu, MD, Vice Chair and Professor of Cardiovascular Surgery at Icahn Mount Sinai and a renowned specialist in heart transplantation.
“Dr. Contreras asked me to see Carlos because he was having severe symptoms of heart failure and she felt he needed a heart transplant,” Dr. Anyanwu says. “He was very limited. He couldn't walk a city block without having to stop a couple of times. He was really in a very advanced stage of heart failure.”
In June 2023, Carlos was again admitted to the ICU. “He was in a low cardiac output state, where his organs were not getting enough blood. He had also developed severe pulmonary hypertension, which means the blood pressure inside the lungs was very high,” Dr. Anyanwu explains.
Pulmonary hypertension can be a serious roadblock to a successful heart transplant. “When the blood pressure in the lungs is very high, it's risky to perform a transplant because the new heart is not able to pump against the pressure in the lungs and it can fail,” Dr. Anyanwu explains.
Dr. Anyanwu and his team placed Carlos on a left ventricular assist device to help his heart pump blood to the body, and to reduce the blood pressure in the lungs. However, he still needed to stay in the ICU until a heart became available for transplant. During the next few months, he learned to draw to help pass the time and created cartoons for the staff and for his family.
“Everybody thought he was a marvel! He’s an amazing artist,” says Dr. Anyanwu. “He drew over 100 cartoons while he was in the intensive care unit, to keep all of us happy. He drew topical cartoons about care in the ICU, cartoons about politics, the environment, they could be about anything.”
Dr. Contreras says, “This was his way to cope with this situation. We all brought him pencils. Seeing him every day was a joy.”
A complicated transplant
There were three occasions where a heart was available for transplant, but the surgery was canceled at the last minute due to technical or viability issues. Nursing staff at the ICU were clearly upset on Carlos’ behalf. “On one occasion when the transplant was canceled, the head nurse taking care of me that night suddenly disappeared,” Carlos recalls. “When she came into the room the next day, she said ‘Carlos, why does this keep happening to you? Can I give you a hug?’ and she literally started sobbing—it was wrenching.”
On September 11, 2023, a viable heart was finally available, and Carlos underwent his heart transplant.
“It was a complicated transplant operation,” Dr. Anyanwu says. “When we went in to perform the surgery, the pressures in the lungs were still very high. So we placed a temporary heart pump, a right ventricular assist device, to take the strain of the high pressure off the new heart. We were then able to gradually let the new heart do more of the work and took out the device after three days. After that, the heart was now used to the high pressures of the lungs, and he made a good recovery.”
Carlos was discharged from hospital on November 16, and has been making steady progress. He remembers with gratitude how the nursing staff went the extra mile to help and support him while he was in the ICU. “There was so many wonderful staff, and I remember so many of them. They would not take their breaks to be in the room with me and would say that they liked spending time with me. Even when they transferred me to the Seventh Floor after the heart transplant, the nurses would show up before they went home. They really would go out of their way.”
Carlos came back to see the ICU staff on December 25 and brought 20 boxes of chocolates. He recalls, “They said ‘Oh Carlos, this is great! You came on Christmas Day!’ It was really nice seeing a lot of people that I hadn’t seen in a long time.”
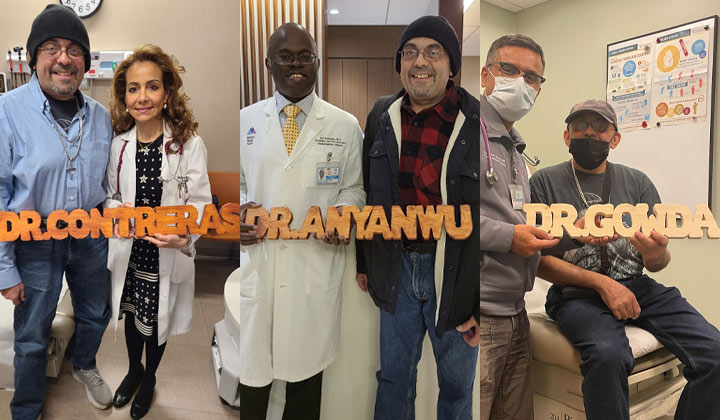
For Dr. Anyanwu, Dr. Contreras, and Dr. Gowda, Carlos made intricate wood carvings of each of their names and gave them as gifts to thank them for their care. He says of Dr. Anyanwu, “I think he's wonderful. He’s irreplaceable—he saved my life. And I knew he was really trying his best from the start. He is just like my savior.”