New Study Shows Novel Anticoagulation Therapy Fails to Improve Angioplasty Patient Outcomes
A novel therapy that allows doctors to turn the body's blood-clotting ability off and on in a more controlled way showed similar efficacy to established anticoagulants in patient undergoing angioplasty, without improvement in major/severe bleeding when compared with bivaliridin, according to an analysis of data from a terminated Phase III trial presented at the American College of Cardiology's 64th Annual Scientific Session.
The study was officially halted in August 2014 due to an excess of severe allergic reactions, so authors caution that the data should be considered exploratory given the early termination.
Before the trial was stopped, 3,232 patients undergoing angioplasty, a procedure to open or widen blocked coronary arteries, at 225 hospitals in 17 countries including North America and Europe were enrolled in the study, which was designed to compare the safety and efficacy of the REG1 Anticoagulation System and bivalirudin—a commonly used anticoagulant—in a total of 13,200 patients. Patients were equally randomized to the bivalirudin or REG1 in an open-label fashion and data was collected at 3 and 30 days.
The analysis revealed there were no differences between patients receiving REG1 vs. bivalirudin in terms of the study's primary efficacy endpoint – a composite of all-cause death, heart attack, stroke or urgent revascularization, which was reported in 6.7 percent of patients in the REG1 arm and 6.4 percent of patients receiving bivalirudin three days after angioplasty. Efficacy was still comparable at 30 days. The REG1 system also did not show a benefit in the primary safety endpoint of bleeding compared to bivalirudin. Using a validated bleeding scale, patients receiving REG1 had a 0.4 percent rate of severe or fatal bleeding compared to 0.1 percent with patients who were given bivalirudin for anticoagulation. However, moderate to severe bleeding was significantly higher in the REG 1 group compared with bivalirudin. Serious allergic reactions were seen in 10 out of 1,605 patients in the REG1 arm, one of which was fatal and the others were anaphylactic reactions. There was only one patient in the bivalirudin group who had a serious allergic event.
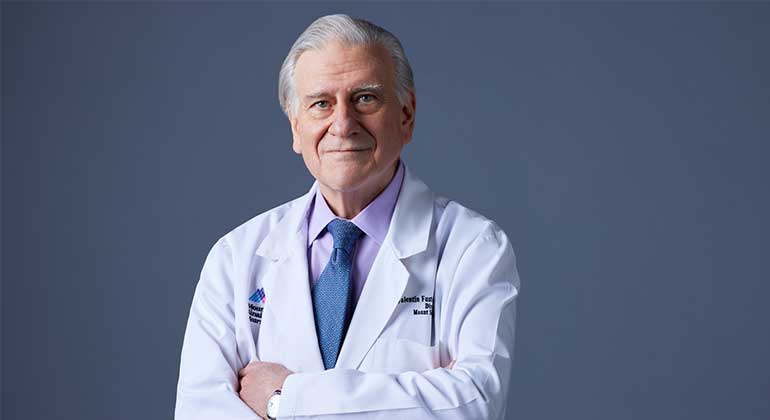
"This anticoagulant system is associated with infrequent, but an unacceptably high rate of severe allergic reactions," said Roxana Mehran, MD, Director of Interventional Cardiovascular Research and Clinical Trials at Mount Sinai Heart at The Mount Sinai Hospital and professor of Medicine in Cardiology at Icahn School of Medicine at Mount Sinai, and one of the principal investigators of this trial. There is ongoing research to determine the exact cause of the allergic reactions, and Mehran said she hopes this does not deter the search for novel anticoagulants for use in this patient population.
When patients undergo angioplasty, they need medications to thin the blood to avoid clots from forming in the coronary artery, which can result in stroke, heart attack, repeat procedures, or even death. However, it's a fine line between preventing blood clots and exposing patients to potentially dangerous bleeding.
"It's the Achilles heal in cardiovascular medicine – how do we protect patients against any kind of blood clotting without exposing them to a higher risk of bleeding?" said Mehran. "We are constantly refining the antithrombotic therapies we use during PCI, and this seemed promising."
More than one million people in the United States undergo angioplasty each year. Roughly 0.6 to 4.8 percent of these will die, 0.2 percent will suffer with a stroke and up to 6 percent will suffer vascular complications in hospital. About 5.8 percent of people will also suffer bleeding related complications within 72 hours of angioplasty.
Mehran said the ideal anticoagulant is one that works fast, has a predictable dose, can efficiently stop clots from forming on top of catheters, but can also be quickly reversed. Blood clotting in the body is regulated by a set of proteins in the blood, called coagulation factors, and platelets. The REG1 system uses a molecule called pegnivacogin that binds to the blood coagulation Factor IXa receptor to deactivate blood clotting, and anivamersen, an active control agent that rapidly reverses the anticoagulant effect, helping patients' blood clotting activity quickly return to normal.
"Within seconds of giving the reversal agent anticoagulation is nearly completely reversed because it looks for its friend and grabs it off the receptor immediately," said Mehran. "With a technique like this, we could provide blood thinning as needed and then take it away immediately after finishing angioplasty." But, she said, further improvements are needed in its safety profile.
This study was funded by Regado Biosciences Inc., the maker of the REG1 system. Mehran has served on scientific advisory board for Regado Biosciences.
The study was presented at ACC 2015 as the abstract: "A Randomized, Open-Label, Multi-Center, Active-Controlled, Parallel Group Study To Determine the Efficacy and Safety of the REG1 Anticoagulation System Compared to Bivalirudin in Patients Undergoing Percutaneous Coronary Intervention."
The ACC's Annual Scientific Session brings together cardiologists and cardiovascular specialists from around the world each year to share the newest discoveries in treatment and prevention. Follow @ACCMediaCenter and #ACC15 for the latest news from the meeting.
The American College of Cardiology is a 49,000-member medical society that is the professional home for the entire cardiovascular care team. The mission of the College is to transform cardiovascular care and to improve heart health. The ACC leads in the formation of health policy, standards and guidelines. The College operates national registries to measure and improve care, provides professional medical education, disseminates cardiovascular research and bestows credentials upon cardiovascular specialists who meet stringent qualifications. For more information, visit acc.org.
About the Mount Sinai Health System
Mount Sinai Health System is one of the largest academic medical systems in the New York metro area, with 48,000 employees working across seven hospitals, more than 400 outpatient practices, more than 600 research and clinical labs, a school of nursing, and a leading school of medicine and graduate education. Mount Sinai advances health for all people, everywhere, by taking on the most complex health care challenges of our time—discovering and applying new scientific learning and knowledge; developing safer, more effective treatments; educating the next generation of medical leaders and innovators; and supporting local communities by delivering high-quality care to all who need it.
Through the integration of its hospitals, labs, and schools, Mount Sinai offers comprehensive health care solutions from birth through geriatrics, leveraging innovative approaches such as artificial intelligence and informatics while keeping patients’ medical and emotional needs at the center of all treatment. The Health System includes approximately 9,000 primary and specialty care physicians and 10 free-standing joint-venture centers throughout the five boroughs of New York City, Westchester, Long Island, and Florida. Hospitals within the System are consistently ranked by Newsweek’s® “The World’s Best Smart Hospitals, Best in State Hospitals, World Best Hospitals and Best Specialty Hospitals” and by U.S. News & World Report's® “Best Hospitals” and “Best Children’s Hospitals.” The Mount Sinai Hospital is on the U.S. News & World Report® “Best Hospitals” Honor Roll for 2025-2026.
For more information, visit https://www.mountsinai.org or find Mount Sinai on Facebook, Instagram, LinkedIn, X, and YouTube.

Mount Sinai Launches Cardiac Catheterization Artificial Intelligence Research Lab
Sep 15, 2025 View All Press Releases
Mount Sinai Surgeons Perform First Heart-Liver-Kidney Transplants in New York State
May 20, 2025 View All Press Releases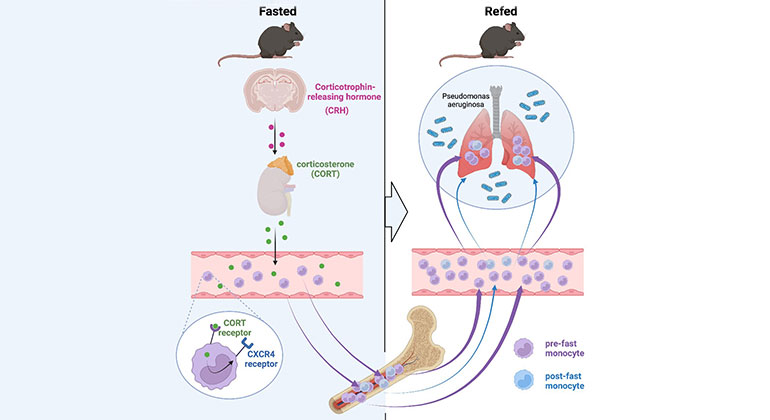
Skipping Breakfast May Compromise the Immune System
Feb 23, 2023 View All Press Releases