Crohn disease - discharge
Inflammatory bowel disease - Crohn disease - discharge; Regional enteritis - discharge; Ileitis - discharge; Granulomatous ileocolitis - discharge; Colitis - discharge
Crohn disease is a disease where parts of the digestive tract become inflamed. It is a form of inflammatory bowel disease.
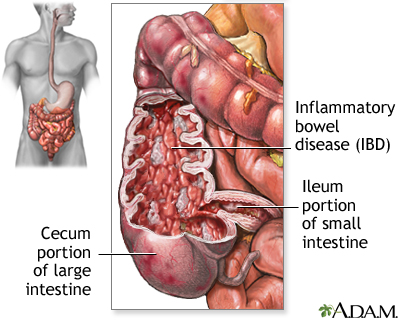
Crohn disease, also called regional enteritis, is a chronic inflammation of the intestines which is usually confined to the terminal portion of the small intestine, the ileum. Ulcerative colitis is a similar inflammation of the colon, or large intestine. These and other IBDs (inflammatory bowel disease) have been linked with an increased risk of colorectal cancer.
Living with Crohn's disease can be a constant gamble, hoping this won't be the day when your disease flares up. Crohn's disease is a type of inflammatory bowel disease. It's caused by a malfunction in the body's immune system. Normally, the immune system protects against bacteria and other foreign invaders. But in people with Crohn's disease, it mistakenly attacks the intestines, causing them to swell up and thicken. As a result, people with Crohn's disease have bouts of severe abdominal pain, diarrhea, and pain with bowel movements. They can lose their appetite, feel tired, and lose weight without meaning to. Some have severe mouth sores. If you've been experiencing any of these symptoms, your doctor can test for Crohn's with a colonoscopy using a scope to look at your colon from the inside. A wireless video capsule may be swallowed to look at the small intestine. Blood tests or other imaging studies may be needed as well. If you're concerned about Crohn's, stop smoking. Smoking can increase your chance of getting Crohn's disease and once you have it smoking can make the condition worse. Medicines can help with the symptoms of Crohn's disease. There are medicines to control diarrhea, and pain relievers to help with abdominal cramps. There are also medicines that quiet the overactive immune response that causes Crohn's. Changing your diet may make a big difference in preventing or reducing symptoms. But as diet that works well for you may be different than the one that works for others. Eating several small meals a day instead of three big ones prevents your intestines from having to process large amounts of food at once. Your doctor may also recommend that you drink lots of water, and avoid high-fiber and high-fatty foods, as well as any foods that you know make you gassy, perhaps beans or broccoli. You may also need to take iron, B12, and other vitamin and mineral supplements if your Crohn's is preventing you from getting enough nutrients through your diet. If medicines and diet changes aren't enough to reduce your symptoms, and you develop bleeding or an infection in your intestines, you may need a procedure called a bowel resection to remove the diseased part of your intestines. This procedure won't cure Crohn's, but it can help control the complications of the disease. If you're experiencing Crohn's symptoms, like stomach pain, severe diarrhea, or unplanned weight loss, call your doctor. Although there's no cure for Crohn's, treatments can relieve some of the uncomfortable symptoms, prevent complications, helping improve your quality of life.
When You're in the Hospital
You were in the hospital because you have Crohn disease. This is an inflammation of the surface and deep layers of the small intestine, large intestine, or both. Less often, other parts of your gastrointestinal tract can be affected.
You may have had exams, lab tests, and x-rays. The inside of your rectum and colon may have been examined using a flexible tube (colonoscopy). A sample of your tissue (biopsy) may have been taken.
You may have been asked not to eat or drink anything and have been fed only through an intravenous line. You may have received special nutrients through a feeding tube.
You may have also started taking new medicines to treat your Crohn disease.
Surgeries you may have had include repair of a fistula, small bowel resection, or ileostomy.
What to Expect at Home
After a flare-up of your Crohn disease, you may be more tired and have less energy than before. This should get better. Ask your health care provider about any side effects from your new medicines. You should see your provider regularly. You may also need frequent blood tests, especially if you are on new medicines.
If you went home with a feeding tube, you will need to learn how to use and clean the tube and your skin where the tube enters your body.
Diet
When you first go home, you may be asked to drink only liquids or eat different foods from what you normally eat. Ask your provider when you can start your regular diet.
You should eat a well-balanced, healthy diet. It is important that you get enough calories, protein, and important nutrients from a variety of food groups.
Certain foods and drinks can make your symptoms worse. These foods may cause problems for you all the time or only during a flare-up. Try to avoid foods that make your symptoms worse.
- If your body does not digest dairy foods well, limit dairy products. Try low-lactose cheeses, such as Swiss and cheddar, or an enzyme product, such as Lactaid, to help break down lactose. If you must stop eating dairy products, talk with a dietitian about getting enough calcium. Some experts believe that you should avoid dairy products altogether until you are tolerating your regular diet.
- Too much fiber may make your symptoms worse. Try baking or stewing fruits and vegetables if eating them raw bothers you. Eat low-fiber foods if that does not help enough.
- Avoid foods that are known to cause gas, such as beans, spicy food, cabbage, broccoli, cauliflower, raw fruit juices, and fruits, especially citrus fruits.
- Avoid or limit alcohol and caffeine. They may make your diarrhea worse.
Eat smaller meals, and eat more often. Drink plenty of liquids.
Ask your provider about extra vitamins and minerals you may need:
- Iron supplements (if you have iron deficiency anemia)
- Nutritional supplements
- Calcium and vitamin D supplements to help keep your bones strong
- Vitamin B-12 shots, to prevent anemia
Talk with a dietitian, especially if you lose weight or your diet becomes very limited.
Stress
You may feel worried about having a bowel accident, embarrassed, or even feel sad or depressed. Other stressful events in your life, such as moving, job loss, or the loss of a loved one, can cause problems with your digestion.
These tips help you to manage your Crohn disease:
- Join a support group. Ask your provider about groups in your area.
- Exercise. Talk with your provider about an exercise plan that is right for you.
- Try biofeedback to reduce muscle tension and slow your heart rate, deep breathing exercises, hypnosis, or other ways to relax. Examples include doing yoga, listening to music, reading, or soaking in a warm bath.
- See a mental health professional for help if necessary.
Drug Treatment
Your provider may give you some medicines to help relieve your symptoms. Based on how bad your Crohn disease is and how you respond to treatment, your provider may recommend one or more of these medicines:
- Anti-diarrhea medicines can help when you have very bad diarrhea. Loperamide (Imodium) can be bought without a prescription. Always talk to your provider before using these medicines.
- Fiber supplements may help your symptoms. You can buy psyllium powder (Metamucil) or methylcellulose (Citrucel) without a prescription. Ask your provider about these.
- Always talk to your provider before using any laxative medicines.
- You may use acetaminophen (Tylenol) for mild pain. Medicines such as aspirin, ibuprofen (Advil, Motrin), or naproxen (Aleve, Naprosyn) may make your symptoms worse. Talk to your provider about medicines you can use. You may need a prescription for stronger pain medicines.
There are many types of medicines that can help prevent or treat attacks of your Crohn disease.
When to Call the Doctor
Contact your provider if you have:
- Persistent or recurring cramps or pain in your lower stomach area
- Bloody diarrhea, often with mucus or pus
- Diarrhea that cannot be controlled with diet changes and medicines
- Weight loss (in everyone) and failure to gain weight (in children)
- Rectal bleeding, drainage, or sores
- Fever that lasts more than 2 or 3 days, or a fever higher than 100.4°F (38°C) without an explanation
- Nausea and vomiting that lasts more than a day
- Skin sores or lesions that do not heal
- Joint pain that keeps you from doing your everyday activities
- Side effects from any drugs prescribed for your condition
References
Ananthakrishnan AN, Reguerio MD. Management of inflammatory bowel disease. In: Feldman M, Friedman LS, Brandt LJ, eds. Sleisenger and Fordtran's Gastrointestinal and Liver Disease. 11th ed. Philadelphia, PA: Elsevier; 2021:chap 116.
Lichtenstein GR. Inflammatory bowel disease. In: Goldman L, Schafer AI, eds. Goldman-Cecil Medicine. 26th ed. Philadelphia, PA: Elsevier; 2020:chap 132.
Rezapour M, Avalos D, Damas OM. Inflammatory bowel disease. In: Kellerman RD, Rakel DP, Heidelbaugh JJ, Lee EM, eds. Conn's Current Therapy 2023. Philadelphia, PA: Elsevier 2023:236-243.
Version Info
Last reviewed on: 11/3/2022
Reviewed by: Michael M. Phillips, MD, Emeritus Professor of Medicine, The George Washington University School of Medicine, Washington, DC. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.
