Precision Urology
At Mount Sinai, our Precision Urology™ approach to diagnosing prostate cancer involves integrating multiple variables and imaging data in a decision-support system. This collaboration is key in assuring men with prostate cancer of our commitment to a patient-centric, personalized diagnostic approach and excellent outcome, while minimizing the side effects of treatment. Precision Urology, developed by Ashutosh (Ash) K. Tewari, MD, Chair of the Department of Urology and world renowned robotic prostate cancer surgeon, reflects our use of advanced technologies and incorporation of molecular and genomic analysis to identify markers of aggressive disease. This allows us to rigorously stage diseases to determine if intervention is needed and if so, tailor the treatment accordingly.
Advanced robotic technique (ART) is highly successful in curing prostate cancer while minimizing side effects in select patients. We have developed and refined ART over the past decade, based on the thousands of surgeries we have performed, our discoveries in prostate anatomy, and other recent research.
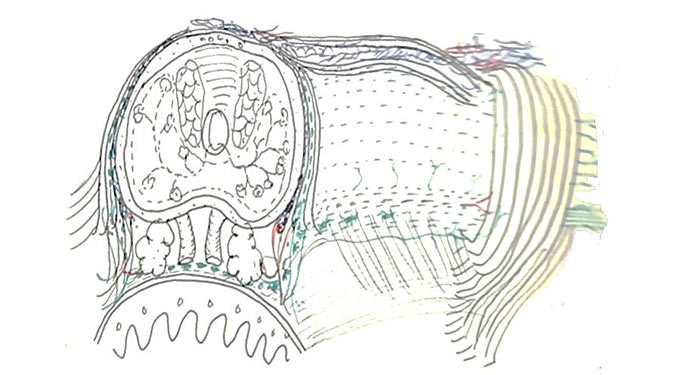
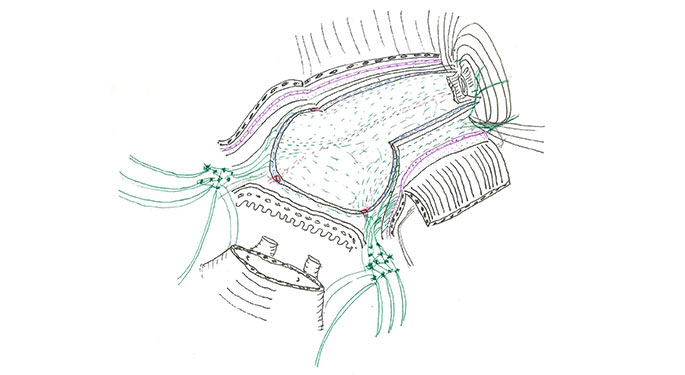
ART is individualized, reflecting your anatomy, cancer location, and neural structure. We routinely make anatomical drawings of prostates that we will operate on, to map out the cancer’s special relationships to the fascia, muscles, and nerves that surround the prostate. By drawing the anatomy of individual cases, we continue to fine-tune ART and improve cancer control while sparing nerves.
The crux of the ART technique is the delicate removal of the prostate from the top of the nerve hammock with maximum clearance for preserving sexual and urinary function. Not only do we avoid handling nerves, but we are able to monitor oxygenation of the nerves during this phase, leaving the nerves healthier and more numerous.
Distinctive features of this approach are:
Precise diagnosis through state-of-the-art evaluation. We use targeted biopsy to diagnose prostate cancer. This technique fuses highly detailed magnetic resonance imaging (MRI) with real-time ultrasound using the Artemis device. The procedure typically takes 15 to 20 minutes in our office under local anesthesia. It provides highly accurate information about the location of the cancer and its relation to nerves and sphincters.
Cancer control. ART leaves fewer cancer cells in the body than other robotic techniques. Consequently, there is less need for radiation and hormone treatment after surgery, and there is less reason to be concerned about future issues. Our program is one of the few in the world where pathologists are on stand-by to provide real-time interpretation of the entire prostate margin, rather than small pieces of tissue in the lab.
High rates of erectile function recovery. Our aim is to preserve every nerve fiber responsible for the fine balance between erection, organism, and bladder function. ART allows for stronger erections and orgasms, a reduction in penile shrinkage, and a decrease in the risk of involuntary release of the urine at the moment of orgasm.
Faster return to urinary continence. Our approach incorporates a novel surgical technique to minimize or prevent urinary leakage, even with exertion, and provide a strong urinary stream. It involves reconstruction of the supporting structures responsible for urinary continence that are typically either removed or disorganized during excision of the prostate. Fully 97 percent of our patients who are continent before surgery are continent within 18 months after the procedure.
ART patients and their families benefit from faster convalescence, shorter hospital stays, smaller incisions with less scarring, significantly decreased blood loss during surgery, and less pain afterward. Most of our patients return home within 24 hours of their robotic surgery.
Our arsenal of Precision Urology tools and techniques include the following:
Precise MD™
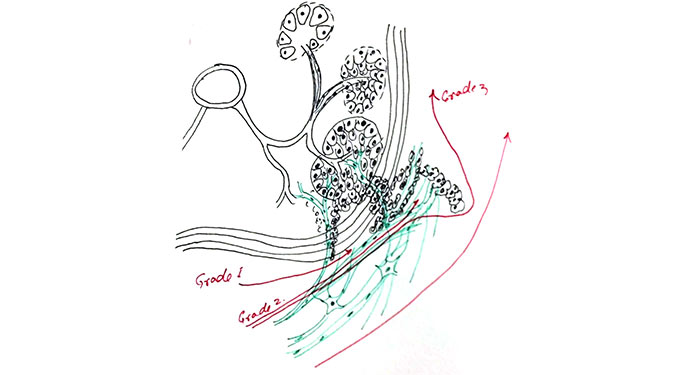
Precise MD™ is developing new approaches to characterizing an individual’s cancer by combining multiple data sources and analyzing them with mathematical algorithms, offering a more sophisticated alternative to standard approaches. With respect to prostate cancer, we are partnering with the Department of Pathology’s Center for Computational and Systems Pathology to advance the Precise MD approach and mathematically characterize the Gleason score, a grading system that has been used since the 1960s to guide prostate cancer patient’s treatment options and establish the prognosis. In its initial phase, Precise MD will complete a test used to analyze patients, who have had prostatectomies at theMount Sinai Health System, to help determine who is likely to have a recurrence of cancer and may need additional therapy such as chemotherapy. A second, higher-impact test will follow in 2017, which will be used to characterize prostate cancer in newly diagnosed patients.
Artemis
Our arsenal of Precision Urology tools and techniques include Artemis, an imaging device that allows 3D prostate visualization and tracking. By fusing multi-parametric MRI with real-time ultrasound, abnormal or suspicious areas seen on the MRI can be tracked and targeted during a prostate biopsy. Artemis offers sophisticated recording of actual biopsy sites sampled, which can be reviewed at any time. Mount Sinai is one of a few facilities in New York City with an Artemis device.
3 Tesla (3T) Multiparametric Magnetic Resonance Imaging
3T MRI is a state-of-the-art, non-invasive imaging modality that facilitates diagnosing, staging, and pre-operative planning for prostate cancer. Magnetic waves create images of the prostate and surrounding tissue. Using advanced computer algorithms, we can process images to predict where prostate cancer lesions are located.
NeuroSAFE™
NeuroSAFE™ allows us to assess the surgical margins for absence or presence of cancer intra-operatively. This helps us perform adequate nerve sparing and remove more tissue, if necessary, to ensure safety.
DNA/RNA Sequencing
We are working to unravel the genetic factors linked to prostate cancer. Genetic screening can pick up mutations in your genetic code that may increase the risk of advanced prostate cancer. We combine genetic information with advanced imaging and immunohistochemistry to determine prostate cancer risk and staging. We design prostate cancer screening plans tailored to your risk profile.