Neuromuscular Disease
Neuromuscular diseases affect the peripheral nervous system, which consists of the nerves, muscles, and the neuromuscular junctions between them, called synapses. The peripheral nervous system enables us to gather information about our environment, send it to the brain for analysis, and carry out the actions the brain chooses. Neuromuscular disease can affect any or all of these processes and can severely impact daily life.
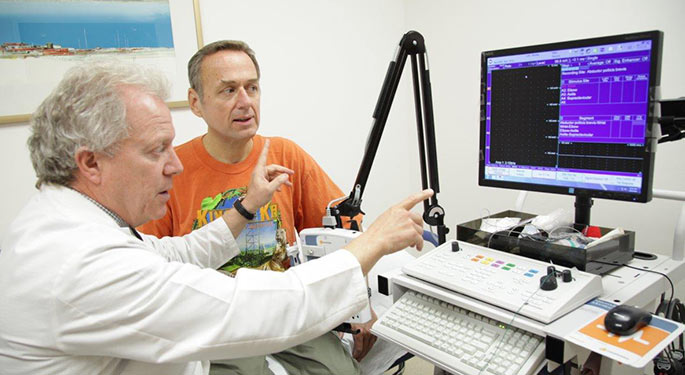
Our Department of Neurology offers you and your loved ones personalized, state-of-the-art care for disorders in neuromuscular transmission, muscle diseases, and peripheral nerve problems. Under the direction of David Simpson, MD, our specialists are highly experienced in diagnosing and managing these disorders, and provide a complete range of testing services using the most advanced techniques and technologies supported by an on-site laboratory. If you have been diagnosed with a neuromuscular disease, we also offer access to clinical trials that explore promising new therapeutics.
About the Neuromuscular System
The peripheral nervous system is made up of several components that allow the body to move and sense the environment. Neuromuscular disease occurs when there is a problem in one of these components:
Nerves
Nerves are similar to cables that transmit electrical impulses to and from the body, to the central nervous system (CNS), which includes our brain and spinal cord. The different types of nerves are:
- Motor nerves supply information from the CNS to the muscles, which enables movement.
- Sensory nerves transmit data from the skin and joints to the CNS, which allow for sensation and balance.
- Autonomic nerves allow the heart, blood vessels, and sweat glands to communicate, which lets the brain control heart rate, blood pressure, and temperature.
Muscles
Our muscular systems facilitate movement. Skeletal muscle is attached to bones and is made up of individual muscle cells. Muscles contract when they receive a chemical signal released from the terminal nerve branch of a motor nerve. Muscle diseases can be caused by genetic or acquired disorders.
Neuromuscular Junction
The neuromuscular junction is a highly specialized gap between the motor nerve terminal and the muscle. As an electrical impulse travels down the motor nerve, a chemical neurotransmitter called acetylcholine travels across the gap to the muscle causing it to contract. Myasthenia gravis is an example of a disorder that affects the neuromuscular junction.



