Mount Sinai’s The Arnhold Institute for Global Health and United Nations Office Release Joint Report on the Essential Role of Community Health Workers in the United States
The Arnhold Institute for Global Health at the Icahn School of Medicine at Mount Sinai and the Office of the United Nations Secretary-General’s Special Envoy for Health in Agenda 2030 and for Malaria today released a special report detailing why community health workers (CHWs) are essential in improving the health of patients by bridging the gap between clinical and community settings. The report, published by a task force of global and domestic experts and frontline leaders, presents a framework for developing sustainable financial and organizational models for CHWs in the context of ongoing changes to the American health care system. Also included is a plan to pilot a sustainable CHW program in Newark, New Jersey, through a partnership among key stakeholders in city and state government, a public hospital, community advocates and the state’s largest health insurer.
CHWs are non-clinical workers who come from the communities of the patients they serve, whose job is to help patients live healthier lives, as well as to help providers better understand and respond to patient needs. While CHWs have existed in the United States for decades, they have not been historically recognized as a core unit of U.S. health infrastructure the way they are in many countries abroad. This is due in large part to the American model of fee-for-service payment for care, which does not incentivize the types of preventive or maintenance support that CHWs often provide. CHW programs have also struggled within a U.S. context because health systems are designed on the basis of clinical care being delivered at hospitals and clinics, leaving many patients unable to comply with the medical advice they receive once they return home.
“We’ve known for a long time that the United States spends more on health care than its peer nations yet obtains poorer outcomes in many key health indicators,” said Prabhjot Singh, MD, PhD, Director of The Arnhold Institute for Global Health, and Chair, Department of Health System Design and Global Health, Icahn School of Medicine at Mount Sinai, and Chair of the Task Force on Sustainable, Effective Community Health Worker Programs in the United States. “It is unacceptable that a person born and raised in Manhattan’s Upper East Side can expect to live, on average, 16 years longer than someone in Bolivar County, Mississippi. Adding to this disconnect is a wide gap between clinical care and communities, leaving the realities of patients’ lives and perspectives out of the care plan.”
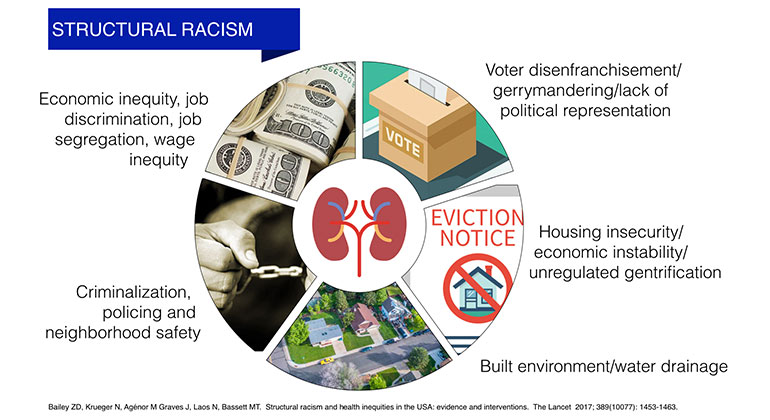
“A growing body of evidence shows that social, economic, genomic and cultural factors can impact an individual’s ability to build and maintain health, and community health workers can change the paradigm of medical care by making this rich context actionable,” said Dr. Singh. “Our findings indicate that with careful construction of the right care models, including all of the organizational and financial infrastructure needed to support them, CHWs can contribute enormous value to patients, communities, and health systems alike.”
The task force identified a number of principles for effective CHW programs, drawn from successful programs in Brazil, India, and Ethiopia.
These principles include:
- Prioritize the patient at the center of care;
- Reflect community needs in every aspect of design;
- Follow clearly defined, evidence-based protocols to meet patient needs;
- Build strong systems to support the service provided by CHWs;
- Select and develop a high-quality workforce;
- Make CHWs an integrated part of the full care team;
- Align programmatic, operational and financial models;
- Be a strong partner to health systems.
“Across the globe we’ve seen the value and impact of community health workers,” said Daniel Palazuelos, MD, MPH, Senior Health and Policy Advisor for Community Health Systems at Partners in Health and a task force member. “When CHWs are effectively selected, trained, supervised, remunerated, and integrated into care delivery teams, they help us understand our patients better, and provide an invaluable extension of care deep into the communities where they live. I marvel at the health impacts we achieve abroad, and then I too often lament that the same is not available for my patients in Boston. Working with CHWs is simply a better way of practicing medicine.”
“RWJBarnabas Health is excited to test the community health worker (CHW) model, particularly in Newark, which provides tremendous opportunity to improve access to primary care and foster healthier communities,” said Jennifer Velez, Senior Vice President of Community and Behavioral Health, RWJBarnabas Health.
Additional collaborators on the task force report include Rutgers, the State University of New Jersey; Dalberg Global Development Advisors; Penn Center for Community Health Workers; AdvantageCare Physicians; LSU Health New Orleans School of Public Health; City Health Works; Partners in Health; CityMD; Center for Medicare and Medicaid Innovation; Iora Health; New Jersey Medical School; RWJBarnabas Health; and The MCJ Amelior Foundation.
About The Arnhold Institute for Global Health
The Arnhold Institute for Global Health at the Icahn School of Medicine, Mount Sinai Health System, seeks to improve the health of people and the communities they live in, both in the United States and abroad. The Arnhold Institute serves as a global arm of the Mount Sinai Health System, leading research on the design of more equitable and effective care models that are disseminated through digital products, training systems and input on policy design.
About the Office of the UN Secretary-General’s Special Envoy for Health in Agenda 2030 and for Malaria, Ray Chambers
Ray Chambers serves as the UN Secretary-General’s Special Envoy for Health in Agenda 2030 and for Malaria. Under Mr. Chambers’ leadership, the Office has been tasked with catalyzing efforts and commitments required for the successful implementation of the health-related goals in Agenda 2030—which includes ending the epidemics of AIDS, TB, and malaria.
About the Icahn School of Medicine
The Icahn School of Medicine at Mount Sinai is an international leader in medical and scientific training, biomedical research, and patient care. It is the medical school for the Mount Sinai Health System, an integrated health care system which includes seven hospitals and an expanding ambulatory network serving approximately 4 million patients per year.
The School has more than 1,800 students in MD, PhD, and Master’s programs and post-doctoral fellowships; more than 5,600 faculty members; over 2,000 residents and fellows; and 23 clinical and research institutes and 34 academic departments. It is ranked among the highest in the nation in National Institutes of Health funding per principal investigator. The School was the first medical school in the country to create a progressive admissions approach for students who seek early assurance of admission through the FlexMed program.
The Graduate School of Biomedical Science trains PhD and MD/PhD students, and offers master’s-level programs in areas such as genetic counseling, clinical research, biomedical sciences, and public health, and an online master’s degree in health care delivery leadership. The seamless connections between our medical school, graduate school, and hospital campuses provide an extraordinary environment for translating scientific discoveries into clinical treatments.
For more information, visit http://icahn.mssm.edu or find the Icahn School of Medicine at Mount Sinai on Facebook, Twitter, YouTube, and LinkedIn.
About the Mount Sinai Health System
Mount Sinai Health System is one of the largest academic medical systems in the New York metro area, with more than 43,000 employees working across eight hospitals, over 400 outpatient practices, nearly 300 labs, a school of nursing, and a leading school of medicine and graduate education. Mount Sinai advances health for all people, everywhere, by taking on the most complex health care challenges of our time — discovering and applying new scientific learning and knowledge; developing safer, more effective treatments; educating the next generation of medical leaders and innovators; and supporting local communities by delivering high-quality care to all who need it.
Through the integration of its hospitals, labs, and schools, Mount Sinai offers comprehensive health care solutions from birth through geriatrics, leveraging innovative approaches such as artificial intelligence and informatics while keeping patients’ medical and emotional needs at the center of all treatment. The Health System includes approximately 7,300 primary and specialty care physicians; 13 joint-venture outpatient surgery centers throughout the five boroughs of New York City, Westchester, Long Island, and Florida; and more than 30 affiliated community health centers. We are consistently ranked by U.S. News & World Report's Best Hospitals, receiving high "Honor Roll" status, and are highly ranked: No. 1 in Geriatrics and top 20 in Cardiology/Heart Surgery, Diabetes/Endocrinology, Gastroenterology/GI Surgery, Neurology/Neurosurgery, Orthopedics, Pulmonology/Lung Surgery, Rehabilitation, and Urology. New York Eye and Ear Infirmary of Mount Sinai is ranked No. 12 in Ophthalmology. U.S. News & World Report’s “Best Children’s Hospitals” ranks Mount Sinai Kravis Children's Hospital among the country’s best in several pediatric specialties.
For more information, visit https://www.mountsinai.org or find Mount Sinai on Facebook, Twitter and YouTube.
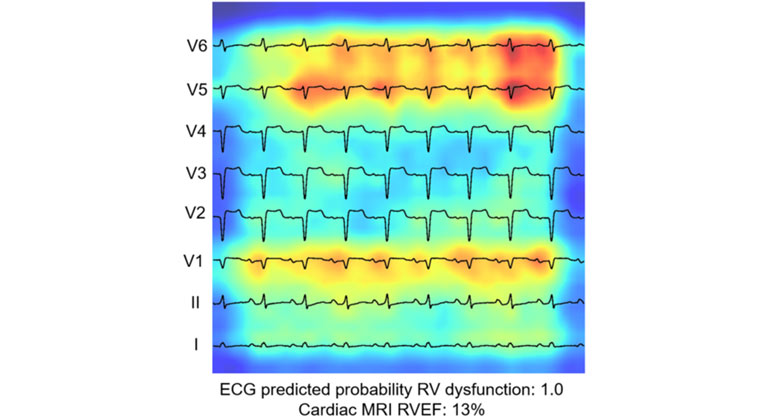
AI-Driven Study Redefines Right Heart Health Assessment With Novel Predictive Model
Jan 04, 2024 View All Press Releases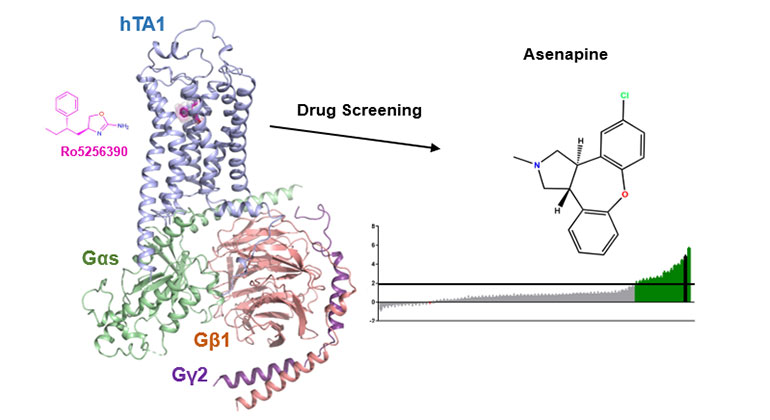
Demystifying a Key Receptor in Substance Use and Neuropsychiatric Disorders
Jan 02, 2024 View All Press Releases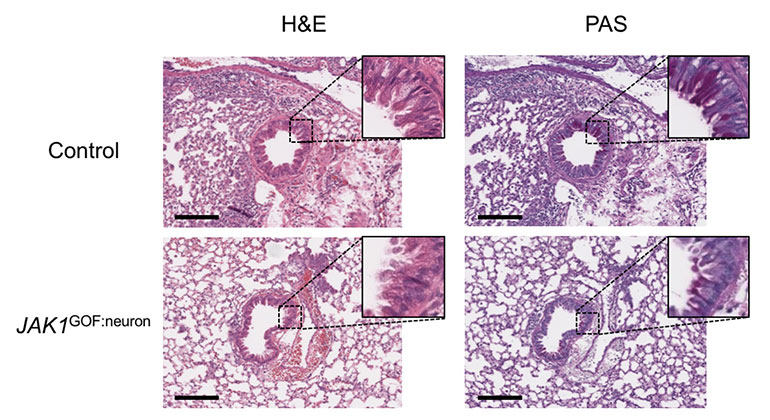
New Insights Revealed On Tissue-Dependent Roles of JAK Signaling in Inflammation
Dec 21, 2023 View All Press Releases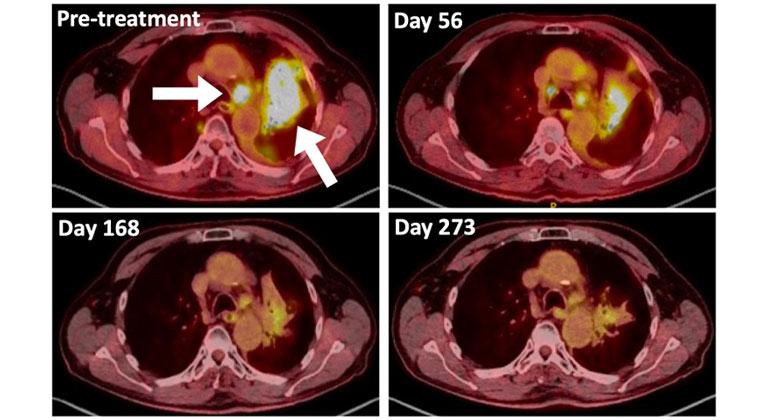
A Type of Allergy Medicine Might Help Treat Lung Cancer, Research Suggests
Dec 06, 2023 View All Press Releases