Study Published in JAMA Finds Tissue Valves As Safe As Mechanical Valves in Middle-Aged Patients Over the Long Term
No significant difference in 15-year survival or stroke rates in younger patients who had aortic valve replacement with bioprosthetic valves compared with mechanical valves.
New Icahn School of Medicine at Mount Sinai research findings published in the October 1 issue of JAMA show there was no significant difference in 15-year survival or stroke rates in patients aged between 50 and 69 years who had aortic valve replacement with bioprosthetic valves (made primarily with biological tissue) compared with mechanical valves. The study results show patients in the bioprosthetic valve group had a greater likelihood of reoperation but a lower likelihood of major bleeding.
About 50,000 patients have aortic valve replacement surgery each year in the United States. In elderly patients, bioprosthetic valves pose a low lifetime risk of needing additional surgeries to address structural degeneration and avert many of the complications associated with mechanical valves; bioprosthetic valves are therefore recommended in patients older than 70 years. Less clear is the best prosthesis type for younger patients because they see higher failure rates of bioprosthetic valves.
"Our study findings support the choice of tissue valves in middle-aged patients who need aortic valve replacement," says Joanna Chikwe, MD, Associate Professor in the Department of Cardiovascular Surgery at Icahn School of Medicine at Mount Sinai and the study's lead author. "Our new evidence may help patients who want to avoid the complications and lifestyle limitations associated with mechanical valves."
"This is one of the largest studies to date on the long-term outcomes of treatment of patients with aortic valve replacement," says the study's senior author Natalia Egorova, PhD, MPH, Assistant Professor in the Department of Population Health Science and Policy at Mount Sinai. "The previous prospective studies have been underpowered to detect differences in long-term survival and major morbidity in the younger age group that we studied."
The study's authors used a statewide patient database to evaluate differences in long-term survival, stroke, reoperation, and major bleeding episodes after aortic valve replacement according to the type of valve implanted. The analysis included 4,253 patients aged 50 to 69 years who underwent primary isolated aortic valve replacement using bioprosthetic versus mechanical valves in New York State from 1997 through 2004. Median follow-up time was 10.8 years, with a maximum follow-up of 16.9 years.
"Our study findings show that tissue valves are as safe as mechanical valves in this younger patient group," says Mr. Chiang, the study's first author, who is currently a fourth year medical student in the inaugural class of the combined MD/Master of Science in Clinical Research PORTAL program at Mount Sinai.
Fifteen-year survival was 60.6 percent in the bioprosthesis group compared with 62.1 percent in the mechanical prosthesis group. The cumulative incidence of stroke at 15 years was 7.7 percent for patients who received a bioprosthetic valve, compared with 8.6 percent for those who received a mechanical prosthetic valve. These differences were not statistically significant.
Bioprostheses were associated with a significantly higher rate of aortic valve reoperation than mechanical prostheses: the cumulative incidence of aortic valve reoperation at 15 years was 12.1 percent in the bioprosthesis group and 6.9 percent in the mechanical prosthesis group. Mechanical prostheses were associated with a significantly higher rate of major bleeding at 15 years compared with bioprostheses: 13.0 percent for the mechanical prosthesis group vs. 6.6 percent for the bioprosthesis group.
"These outcomes, together with the well-recognized patient dissatisfaction with the prospect of a lifetime of anticoagulation, may partially explain the increasing use of bioprostheses," the authors write.
Mount Sinai study co-authors are David H. Adams, MD, Professor and Chair of Cardiovascular Surgery for the Mount Sinai Health System, and Shinobu Itagaki, MD, a surgical resident on the Integrated Thoracic Surgery Residency Program; and Alan J. Moskowitz, MD, Professor in the Department of Population Health Science and Policy.
About the Mount Sinai Health System
Mount Sinai Health System is one of the largest academic medical systems in the New York metro area, with more than 43,000 employees working across eight hospitals, over 400 outpatient practices, nearly 300 labs, a school of nursing, and a leading school of medicine and graduate education. Mount Sinai advances health for all people, everywhere, by taking on the most complex health care challenges of our time — discovering and applying new scientific learning and knowledge; developing safer, more effective treatments; educating the next generation of medical leaders and innovators; and supporting local communities by delivering high-quality care to all who need it.
Through the integration of its hospitals, labs, and schools, Mount Sinai offers comprehensive health care solutions from birth through geriatrics, leveraging innovative approaches such as artificial intelligence and informatics while keeping patients’ medical and emotional needs at the center of all treatment. The Health System includes approximately 7,300 primary and specialty care physicians; 13 joint-venture outpatient surgery centers throughout the five boroughs of New York City, Westchester, Long Island, and Florida; and more than 30 affiliated community health centers. We are consistently ranked by U.S. News & World Report's Best Hospitals, receiving high "Honor Roll" status, and are highly ranked: No. 1 in Geriatrics and top 20 in Cardiology/Heart Surgery, Diabetes/Endocrinology, Gastroenterology/GI Surgery, Neurology/Neurosurgery, Orthopedics, Pulmonology/Lung Surgery, Rehabilitation, and Urology. New York Eye and Ear Infirmary of Mount Sinai is ranked No. 12 in Ophthalmology. U.S. News & World Report’s “Best Children’s Hospitals” ranks Mount Sinai Kravis Children's Hospital among the country’s best in several pediatric specialties.
For more information, visit https://www.mountsinai.org or find Mount Sinai on Facebook, Twitter and YouTube.
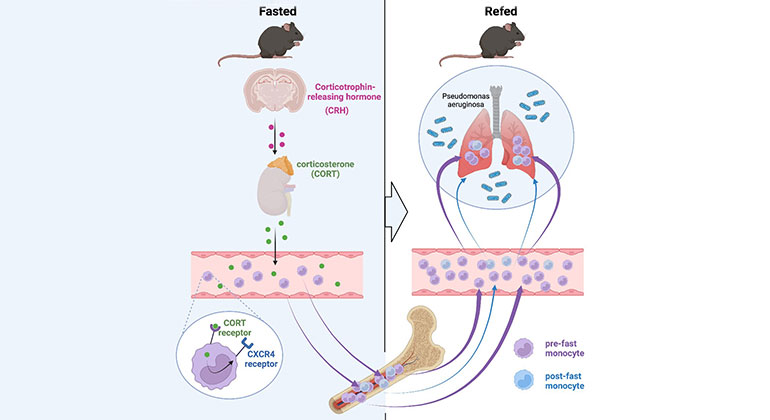
Skipping Breakfast May Compromise the Immune System
Feb 23, 2023 View All Press Releases
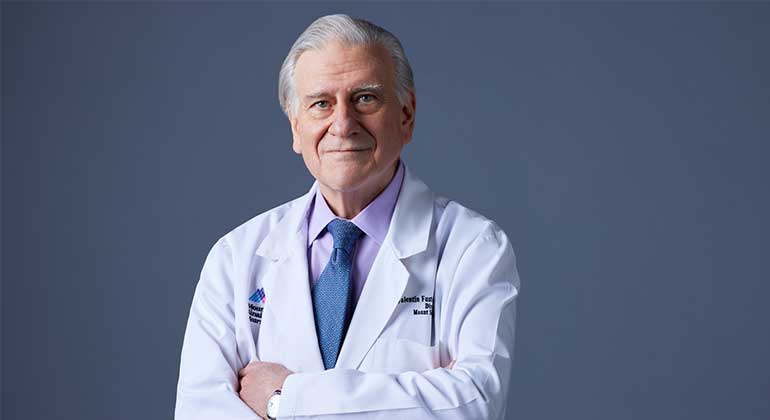
Valentin Fuster, MD, PhD, Receives Prestigious Award from City of Barcelona, Spain
Jan 23, 2023 View All Press Releases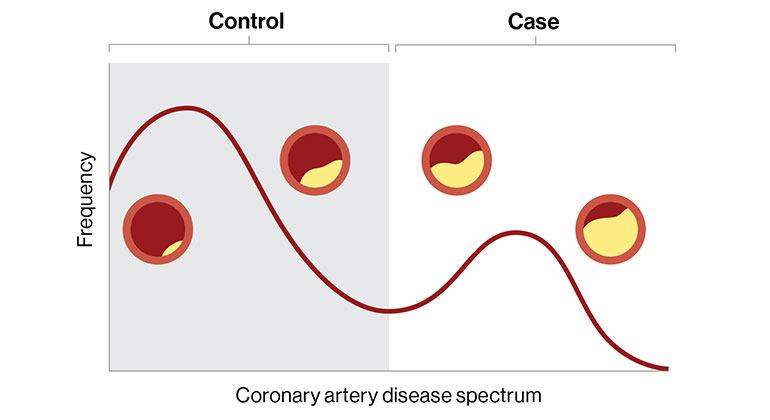
Digital Marker for Coronary Artery Disease Built by Researchers at Mount Sinai
Dec 20, 2022 View All Press Releases
Samin Sharma, MD, Named Director of the Mount Sinai Cardiovascular Clinical Institute
Nov 28, 2022 View All Press Releases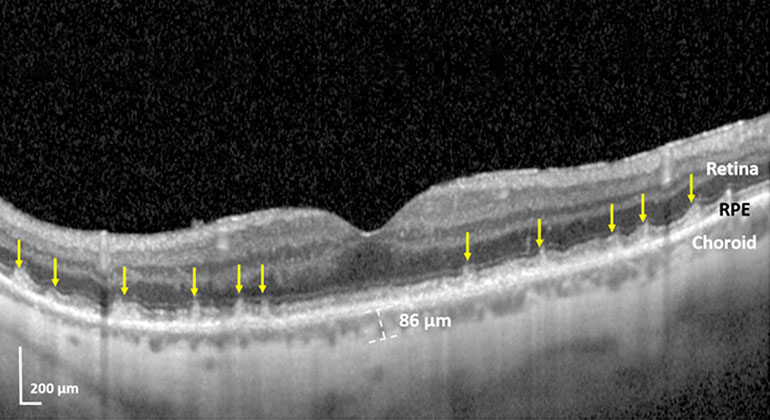
Blinding Eye Disease Strongly Associated With Serious Forms of Cardiovascular Disease
Nov 17, 2022 View All Press Releases