Some Genetic Variations May Be Particularly Difficult To Evaluate Using Current Stem Cell Modeling Techniques
Some heritable but unstable genetic mutations that are passed from parent to affected offspring may not be easy to investigate using current human-induced pluripotent stem cell (hiPSC) modeling techniques, according to research conducted at The Icahn School of Medicine at Mount Sinai and published March 14, in the journal Stem Cell Reports. The study serves to caution stem cell biologists that certain rare mutations, like the ones described in the study, are difficult to recreate in laboratory-produced stem cells.
Stem cell-based disease modeling involves taking cells from patients, such as skin cells, and introducing genes that reprogram the cells into human-induced pluripotent stem cells (hiPSCs). These “master cells” are unspecialized, meaning they can be pushed to become any type of mature cell needed for research, such as skin, liver or brain. The hiPSCs are capable of renewing themselves over a long period of time, and this emerging stem cell modeling technique is helping elucidate the genetic and cellular mechanisms of many different disorders.
“Our study describes how a complex chromosomal rearrangement genetically passed by a patient with psychosis to her affected son was not well recreated in laboratory-produced stem cells,” says Kristen Brennand, PhD, Associate Professor of Genetics and Genomic Sciences, Neuroscience, and Psychiatry at the Icahn School of Medicine, and the study’s senior investigator. “As stem cell biologists dive into studying brain disorders, we all need to know that this type of rare mutation is very hard to model with induced stem cells.”
To investigate the genetic underpinnings of psychosis, the research team used hiPSCs from a mother diagnosed with bipolar disease with psychosis, and her son, diagnosed with schizoaffective disorder. In addition to the normal 46 chromosomes (23 pairs), the cells in mother and son had a very small extra chromosome, less than 1/10th normal size. This microduplication of genes is increasingly being linked to schizophrenia and bipolar disorders, and the extra chromosomal bit, known as a marker (mar) element, falls into the category of abnormally duplicated genes.
For the first time, the Mount Sinai research team tried to make stem cells from adult cells with this type of mar defect. Through the process, they discovered that the mar element was frequently lost during the reprogramming process.
While mar elements in the general population are rare (less than .05 percent in newborn infants), more than 30 percent of individuals with these defects are clinically abnormal, and mar elements are also significantly more likely to be found in patients with developmental delays.
The study found that the mother’s cells were mosaic, meaning some cells were normal while others were not, and the hiPSCs the team created accurately replicated that condition: some were normal and some had the extra mar chromosome. But the technique did not work well with the son’s cells. While all of his cells should have had the mar element, as with his mother, some of the reprogrammed stem cells did not contain the extra bit of chromosome.
“We realized we kept losing the mutation in the stem cells we made, and the inability to recreate cells with mar elements may hamper some neuropsychiatric research,” says Dr. Brennand. “The bottom line is that it is essential that stem cell biologists look for existing mar elements in the cells they study, in order to check that they are retained in the new stem cells.”
Researchers from Baylor College of Medicine, Cold Spring Harbor Laboratory, The University of California, San Diego, McLean Hospital, and Hoffmann-La Roche Ltd., contributed to this research.
The work was supported, in part, by NIH grants R01 MH101454, R21 MH097470, R21 MH1057321, RO1NS058529, R21 MH104505, New York Stem Cell Foundation, Brain and Behavior Young Investigator Grant, the Ellison Foundation, Anonymous Foundation, the Carmela and Menachem Abraham Fund and Team Daniel.
About the Mount Sinai Health System
Mount Sinai Health System is one of the largest academic medical systems in the New York metro area, with more than 43,000 employees working across eight hospitals, over 400 outpatient practices, nearly 300 labs, a school of nursing, and a leading school of medicine and graduate education. Mount Sinai advances health for all people, everywhere, by taking on the most complex health care challenges of our time — discovering and applying new scientific learning and knowledge; developing safer, more effective treatments; educating the next generation of medical leaders and innovators; and supporting local communities by delivering high-quality care to all who need it.
Through the integration of its hospitals, labs, and schools, Mount Sinai offers comprehensive health care solutions from birth through geriatrics, leveraging innovative approaches such as artificial intelligence and informatics while keeping patients’ medical and emotional needs at the center of all treatment. The Health System includes approximately 7,300 primary and specialty care physicians; 13 joint-venture outpatient surgery centers throughout the five boroughs of New York City, Westchester, Long Island, and Florida; and more than 30 affiliated community health centers. We are consistently ranked by U.S. News & World Report's Best Hospitals, receiving high "Honor Roll" status, and are highly ranked: No. 1 in Geriatrics and top 20 in Cardiology/Heart Surgery, Diabetes/Endocrinology, Gastroenterology/GI Surgery, Neurology/Neurosurgery, Orthopedics, Pulmonology/Lung Surgery, Rehabilitation, and Urology. New York Eye and Ear Infirmary of Mount Sinai is ranked No. 12 in Ophthalmology. U.S. News & World Report’s “Best Children’s Hospitals” ranks Mount Sinai Kravis Children's Hospital among the country’s best in several pediatric specialties.
For more information, visit https://www.mountsinai.org or find Mount Sinai on Facebook, Twitter and YouTube.
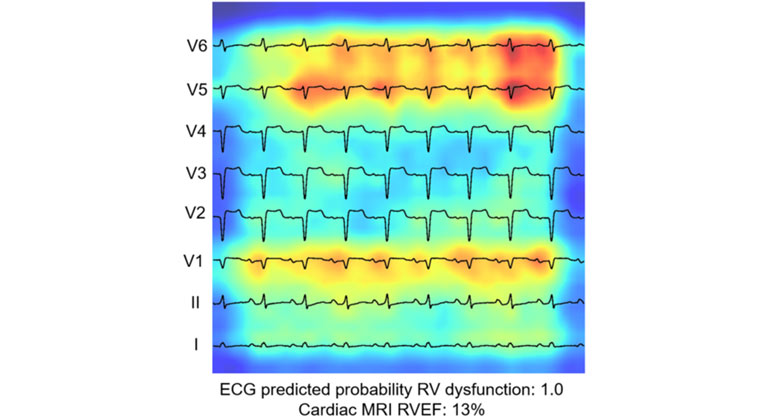
AI-Driven Study Redefines Right Heart Health Assessment With Novel Predictive Model
Jan 04, 2024 View All Press Releases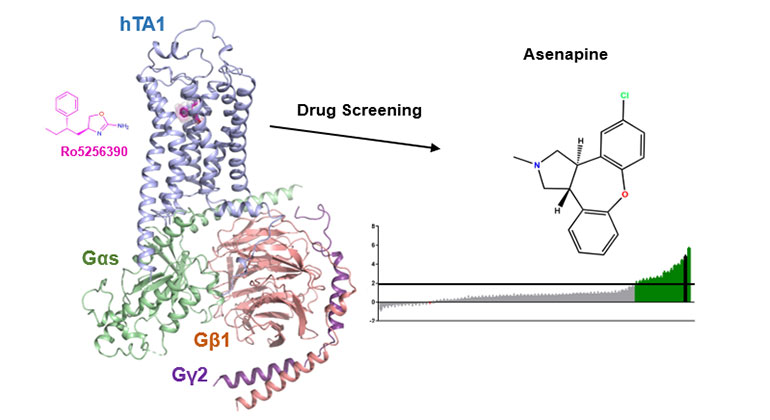
Demystifying a Key Receptor in Substance Use and Neuropsychiatric Disorders
Jan 02, 2024 View All Press Releases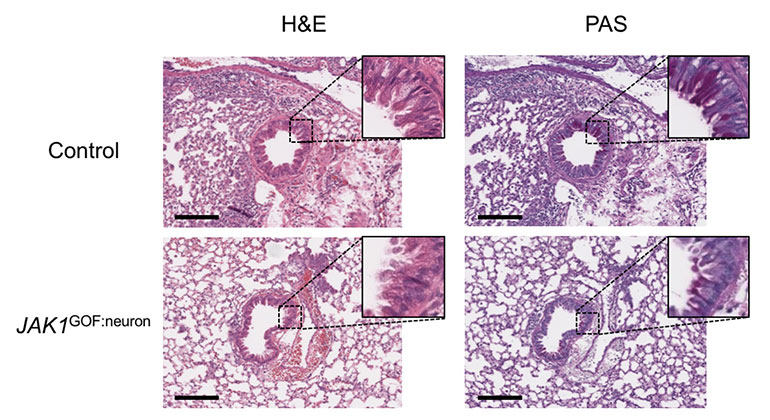
New Insights Revealed On Tissue-Dependent Roles of JAK Signaling in Inflammation
Dec 21, 2023 View All Press Releases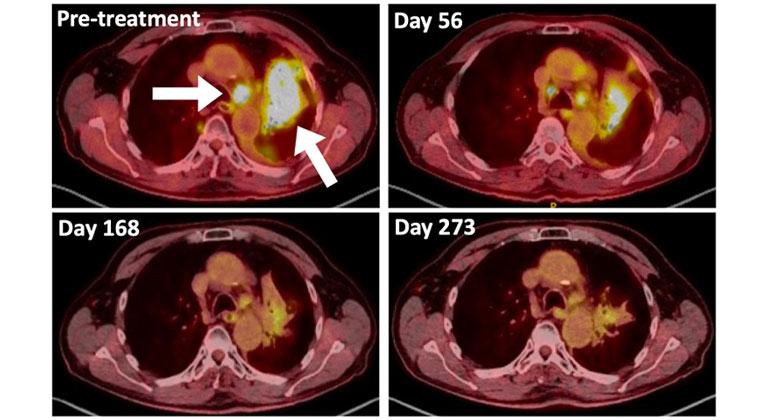
A Type of Allergy Medicine Might Help Treat Lung Cancer, Research Suggests
Dec 06, 2023 View All Press Releases