Mount Sinai Establishes New Pediatric Program for Mood and Anxiety Disorders
Mount Sinai has established a new Pediatric Mood and Anxiety Program to help address the public health crisis of mental illness in children.
The Icahn School of Medicine at Mount Sina has established a new Pediatric Mood and Anxiety Program (PMAP) to help address the public health crisis of mental illness in children. Mood disorders during adolescence are a major concern associated with serious consequences including academic failure, social dysfunction, drug abuse, and suicide—the third leading cause of death in adolescents—but are often overlooked or attributed to an adolescent mood swing.
PMAP will help counsel patients and their families to identify mental illness and provide advanced care for major depression, chronic low moods, bipolar disorder, generalized anxiety disorder, and panic disorder. Patients will have access to a multidisciplinary team of psychiatrists and psychologists as well as cutting-edge clinical trials. PMAP, which is part of the department of Psychiatry at Mount Sinai, is located in renovated space at 1240 Park Avenue and 96th Street.
"The lack of awareness and adequate treatment for psychiatric disorders in youth is nearing epidemic proportions," said Vilma Gabbay, MD, MS, Chief, Child and Adolescent Mood and Anxiety Disorder Program, and one of the nation’s leading clinical experts and researchers in mood disorders in children. "At PMAP, we want to help families recognize the signs of mental illness, dispel the stigma associated with it, and develop new ways to diagnose and treat it.”
Adults with treatment-resistant depression often start having symptoms during adolescence. Dr. Gabbay encourages parents to seek advice early from an expert if they notice long-term changes in their children. “All too often, parents or teachers see a teen begin to act differently in class or at home, and attribute it to an adolescent mood swing, and this is often how cases of mental illness are missed,” said Dr. Gabbay. “Communication between people who observe the behavior and the family is essential. Early diagnosis and treatment are critical.”
Dr. Gabbay and the team at PMAP suggest that parents and educators be on the lookout for the following changes, and to seek help if they last longer than two weeks:
- Changes from typical behavior – social withdrawal, more internal focus
- Acute decrease in academic success – someone who has performed well begins to decline significantly
- Decreased interest in activities that used to be pleasurable
- Decreased ability to concentrate
- Increased irritability and anger
- Ongoing fatigue – someone who’s newly, chronically tired
- Reduced appetite
- Awkward disinhibited behavior – especially if it becomes socially intrusive
- Grandiosity – belief in having super powers
- Reduced level of self-care, including change in hygiene, such as not showering, changing clothes, odor
- Increased preoccupation with a specific event in an unrealistic way
- Decreased need to sleep – not insomnia, but no sleep for several days
PMAP is finding new, multi-dimensional ways to classify mood and anxiety disorders so as to facilitate early identification, personalized treatment, and prevention for young patients. To help identify the underpinning of mood and anxiety disorders in children, PMAP research team uses multidisciplinary investigative approaches that involving immunological and state-of-the-art brain imaging techniques such as proton magnetic resonance (MR) spectroscopy and functional MR imaging.
One important study underway by PMAP researchers involves probing the efficacy of Omega-3FA (fish oil) in the treatment of depressive symptoms in youth ages 12-19. Another study is examining the neurobiology of anhedonia – the loss of pleasure.
“Our team focuses on the development of effective, short-term treatments for childhood anxiety and mood disorders, as well as on the identification of biological markers of these disorders in order to facilitate early detection and prevention,” said Dr. Gabbay.
For more information, visit www.mountsinai.org/pmap.
About The Mount Sinai Medical Center
The Mount Sinai Medical Center encompasses both The Mount Sinai Hospital and Icahn School of Medicine at Mount Sinai. Established in 1968, the Icahn School of Medicine is one of the leading medical schools in the United States, and is noted for innovation in education, biomedical research, clinical care delivery, and local and global community service. It has more than 3,400 faculty in 32 departments and 14 research institutes, and ranks among the top 20 medical schools both in National Institutes of Health (NIH) funding and by U.S. News & World Report.
The Mount Sinai Hospital, founded in 1852, is a 1,171-bed tertiary- and quaternary-care teaching facility and one of the nation’s oldest, largest and most-respected voluntary hospitals. In 2012, U.S. News & World Report ranked The Mount Sinai Hospital 14th on its elite Honor Roll of the nation’s top hospitals based on reputation, safety, and other patient-care factors. Mount Sinai is one of 12 integrated academic medical centers whose medical school ranks among the top 20 in NIH funding and by U.S. News & World Report and whose hospital is on the U.S. News & World Report Honor Roll. Nearly 60,000 people were treated at Mount Sinai as inpatients last year, and approximately 560,000 outpatient visits took place.
For more information, visit http://www.mountsinai.org/.
Find Mount Sinai on:
Facebook: http://www.facebook.com/mountsinainyc
Twitter @mountsinainyc
YouTube: http://www.youtube.com/mountsinainy
# # #
About the Mount Sinai Health System
Mount Sinai Health System is one of the largest academic medical systems in the New York metro area, with more than 43,000 employees working across eight hospitals, over 400 outpatient practices, nearly 300 labs, a school of nursing, and a leading school of medicine and graduate education. Mount Sinai advances health for all people, everywhere, by taking on the most complex health care challenges of our time — discovering and applying new scientific learning and knowledge; developing safer, more effective treatments; educating the next generation of medical leaders and innovators; and supporting local communities by delivering high-quality care to all who need it.
Through the integration of its hospitals, labs, and schools, Mount Sinai offers comprehensive health care solutions from birth through geriatrics, leveraging innovative approaches such as artificial intelligence and informatics while keeping patients’ medical and emotional needs at the center of all treatment. The Health System includes approximately 7,300 primary and specialty care physicians; 13 joint-venture outpatient surgery centers throughout the five boroughs of New York City, Westchester, Long Island, and Florida; and more than 30 affiliated community health centers. We are consistently ranked by U.S. News & World Report's Best Hospitals, receiving high "Honor Roll" status, and are highly ranked: No. 1 in Geriatrics and top 20 in Cardiology/Heart Surgery, Diabetes/Endocrinology, Gastroenterology/GI Surgery, Neurology/Neurosurgery, Orthopedics, Pulmonology/Lung Surgery, Rehabilitation, and Urology. New York Eye and Ear Infirmary of Mount Sinai is ranked No. 12 in Ophthalmology. U.S. News & World Report’s “Best Children’s Hospitals” ranks Mount Sinai Kravis Children's Hospital among the country’s best in several pediatric specialties.
For more information, visit https://www.mountsinai.org or find Mount Sinai on Facebook, Twitter and YouTube.

Mount Sinai Awarded Grant to Assess Music’s Impact on Well-Being, Depression
Apr 27, 2023 View All Press Releases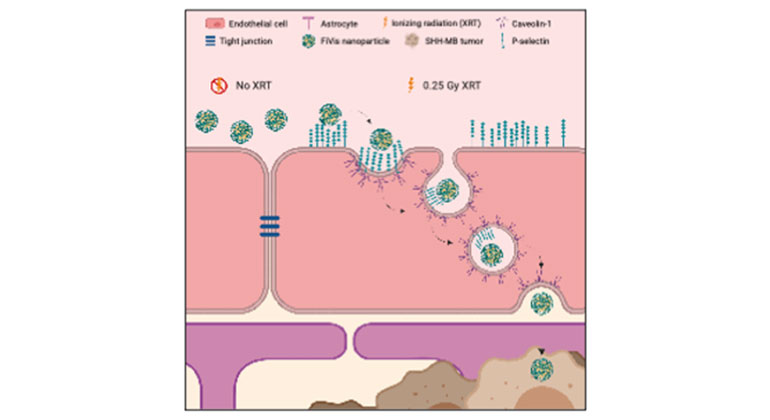
Scientists Develop Novel Approach to Enhance Drug Delivery for Brain Tumors in Children
Mar 02, 2023 View All Press Releases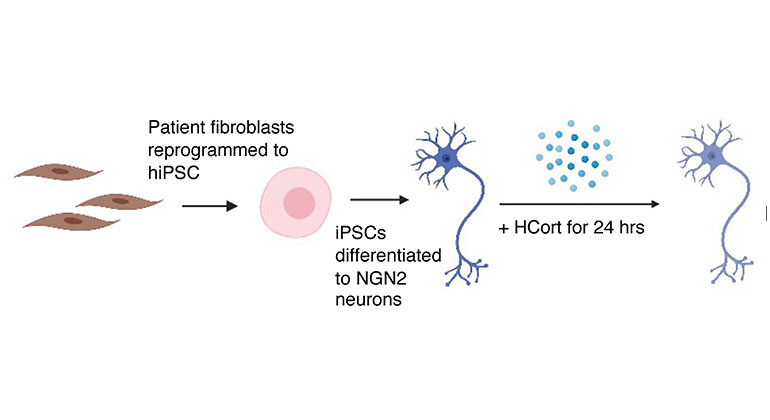
Stem Cell Study Reveals How Neurons From PTSD Patients React to Stress
Oct 20, 2022 View All Press Releases
New Study Suggests Ketamine May Be An Effective Treatment for Children with ADNP Syndrome
Sep 06, 2022 View All Press Releases