Health screening - women - ages 40 to 64
Health maintenance visit - women - ages 40 to 64; Physical exam - women - ages 40 to 64; Yearly exam - women - ages 40 to 64; Checkup - women - ages 40 to 64; Women's health - ages 40 to 64; Preventive care - women - ages 40 to 64
You should visit your health care provider from time to time, even if you are healthy. The purpose of these visits is to:
- Screen for medical issues
- Assess your risk for future medical problems
- Encourage a healthy lifestyle
- Update vaccinations and other preventive care services
- Help you get to know your provider in case of an illness
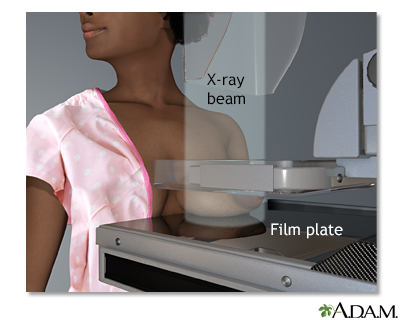
A mammogram is an x-ray picture of the breasts. It is used to find tumors and to help tell the difference between noncancerous (benign) and cancerous (malignant) disease. One breast at a time is rested on a flat surface that contains the x-ray plate. A device called a compressor is pressed firmly against the breast to help flatten out the breast tissue. Each breast is compressed horizontally, then obliquely and an x-ray is taken of each position.

If you're a woman 21 or over, it's important to begin getting regular pelvic examinations to take charge of your health. An important part of this pelvic exam may include a test, called a Pap smear, to detect the often life-threatening disease, cervical cancer, even before it starts. And here's the key, cervical cells become abnormal years before they turn to cancer. That gives an excellent window of opportunity. So, what is a Pap smear? A Pap smear is a microscopic examination of cells scraped from the opening of the cervix. The cervix is the lower part of the uterus, or womb, that opens at the top of the vagina. The test looks for cervical cancer or abnormal cells. Most cervical cancers can be found, and treated early, or even before they start, if women have routine Pap smears and pelvic examinations. For this test, you will lie on a table and place your feet in stirrups. The doctor will insert an instrument called a speculum into the vagina and open it slightly to see inside the vaginal canal. Cells are gently scraped from the cervix area, and sent to a lab for examination. When a Pap smear shows abnormal changes, you will need further testing. The next step depends on the results of the Pap smear, and on your previous history of Pap smears, and risk factors you may have for cervical cancer. You may need a biopsy using a light and a low-powered microscope, called colposcopy. You may also need a test to check for infection with human papilloma virus, or HPV, which can cause cervical cancer. If you are diagnosed with cervical cancer, the doctor will order more tests to determine how you should be treated, and how far the cancer has spread. This is called staging. Treatment will depend on the stage of the cancer, the size and shape of the tumor, your age and general health, and your desire to have children in the future. Early cervical cancer can be treated with surgery to remove the abnormal tissue, or freeze abnormal cells, or burn abnormal tissue. Treatment for more advanced cervical cancer may include radical hysterectomy, removal of the uterus and much of the surrounding tissue, including lymph nodes and the upper part of the vagina. Radiation may be used to treat cancer that has spread beyond the pelvis, or if cancer returns. The woman may also have chemotherapy to kill the cancer if the cervical cancer's advanced. The Pap smear test is not 100% accurate and cervical cancer may be missed in a small number of cases. Fortunately, cervical cancer develops very slowly in most women and follow-up Pap smears should identify worrisome changes in plenty of time for treatment. Make sure your doctor knows about all the medicines you are taking. Some, including estrogen and progestins, may affect the result of your Pap smear. Pap smears can be a wonderful, life saving tool.

Colon cancer is one of the leading causes of cancer-related deaths in the United States. The good news is that earlier diagnosis due to screening tests often leads to a complete cure. Colorectal cancer starts in the large intestine, also known as the colon. Nearly all colon cancers begin as noncancerous, or benign, polyps, some of which may slowly develop into cancer. Screening can detect these polyps and early cancers. Polyps can be removed years before cancer even has a chance to develop. Your doctor can use two types of tools to screen for cancer. The first type is a stool test. Polyps in the colon and small cancers can bleed tiny amounts of blood that you can't see with the naked eye. The most common method to test for the presence of blood is the fecal occult blood test or FOBT. This test checks your stool for small amounts of blood that you may not be able to see. Two other stool tests are the fecal immunochemical test and the stool DNA test. The second type of screening tests involve looking at the lining of the colon. One of these tests is a sigmoidoscopy exam. This test uses a flexible scope to look at the lower portion of your colon. But, because it looks only at the last one-third of the large intestine, it may miss some cancers. So this test is done along with a stool test. A colonoscopy is similar to sigmoidoscopy, but it can see the entire colon. For this test, your doctor will give you instructions for cleansing your bowel. This is called bowel preparation. During the colonoscopy, you’ll receive medicine to make you relaxed and sleepy. Another test your doctor may recommend is a virtual colonoscopy, also called a CT colonography. This test uses a CAT scan and computer software to create a 3-D image of your large intestine. Beginning at age 45, all men and women should have a screening test for colon cancer. Screening options for people with average risk for colon cancer include visual based exams. These could be a colonoscopy every 10 years starting at age 45 or a virtual colonoscopy every 5 years. A Flexible sigmoidoscopy every 5 years or a Flexible sigmoidoscopy every 10 years plus stool testing with FIT done every year. Screening options also include stool based tests. People with average risk should have an FOBT or FIT every year. A colonoscopy is needed if the results are positive, or a Stool DNA test every 1 to 3 years. A colonoscopy is needed if the results are positive. People with certain risk factors for colon cancer may need screening at a younger age, or they may need screening more often. Such people include those with a family history of colon cancer, those with a history of previous colon cancer or polyps, or people with a history of ulcerative colitis or Crohn disease. The death rate for colon cancer has dropped in the past 15 years and this may be due to increased awareness and colon screening. In general, early diagnosis is much more likely to lead to a complete cure.
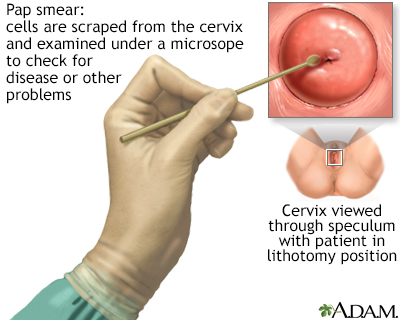
A Pap test is a simple, relatively inexpensive procedure that can easily detect cancerous or precancerous conditions.
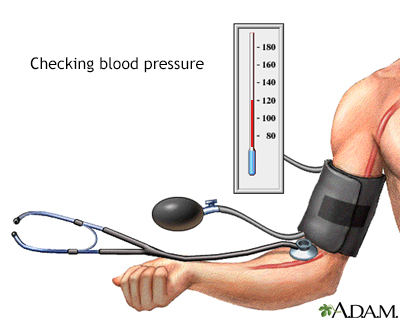
Blood vessels become less elastic with age. The average blood pressure increases from 120/70 to 150/90 and may persist slightly high even if treated. The blood vessels respond more slowly to a change in body position.
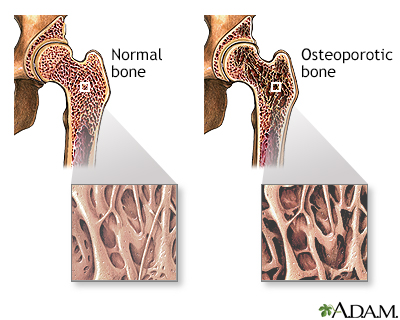
Osteoporosis is a condition characterized by progressive loss of bone density, thinning of bone tissue and increased vulnerability to fractures. Osteoporosis may result from disease, dietary or hormonal deficiency or advanced age. Regular exercise and vitamin and mineral supplements can reduce and even reverse loss of bone density.
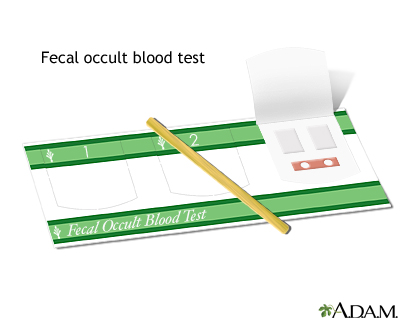
A fecal occult blood test is a noninvasive test that detects the presence of hidden blood in the stool. Blood in the stool that is not visible is often the first, and in many cases the only, warning sign that a person has colorectal disease, including colon cancer.
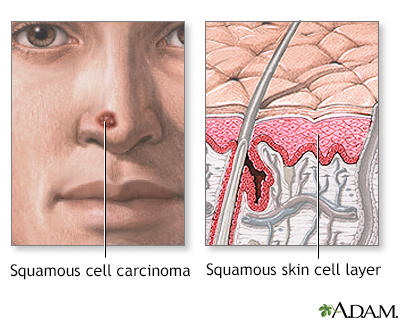
Squamous cell cancer involves cancerous changes to the cells of the middle portion of the epidermal skin layer. It is a malignant tumor, and is more aggressive than basal cell cancer, but still may be relatively slow-growing. It is more likely than basal cell cancer to spread (metastasize) to other locations, including internal organs. Treatment usually involves surgical removal of the tumor along with some surrounding tissue.
Information
Even if you feel fine, you should still see your provider for regular checkups. These visits can help you avoid problems in the future. For example, the only way to find out if you have high blood pressure is to have it checked regularly. High blood sugar and high cholesterol levels also may not have any symptoms in the early stages. A simple blood test can check for these conditions.
There are specific times when you should see your provider or receive specific health screenings. The US Preventive Services Task Force publishes a list of recommended screenings. Below are screening guidelines for women ages 40 to 64.
BLOOD PRESSURE SCREENING
Have your blood pressure checked at least once every year. Watch for blood pressure screenings in your area. Ask your provider if you can stop in to have your blood pressure checked.
Ask your provider if you need your blood pressure checked more often if:
- You have diabetes, heart disease, kidney problems, or are overweight or have certain other health conditions
- You have a first-degree relative with high blood pressure
- You are Black
- Your blood pressure top number is from 120 to 129 mm Hg, or the bottom number is from 70 to 79 mm Hg
- You had high blood pressure during a pregnancy
If the top number is 130 mm Hg or greater or the bottom number is 80 mm Hg or greater, this is considered stage 1 hypertension. Schedule an appointment with your provider to learn how you can reduce your blood pressure.
BREAST CANCER SCREENING
Experts do not agree about the benefits of breast self-exams in finding breast cancer or saving lives. Talk to your provider about what is best for you.
Screening mammogram is recommended for:
- Women ages 40 to 49 every 1 to 2 years. However, not all experts agree about the benefits of having a mammogram when women are in their 40s. Talk to your provider about what is best for you.
- Women ages 50 to 75 every 1 to 2 years, depending on their risk factors, to check for breast cancer.
- Women with a mother or sister who had breast cancer at a younger age should consider yearly mammograms. They should begin screening earlier than the age at which their youngest family member was diagnosed.
If you have other risk factors for breast cancer, your provider may recommend a MRI scan for screening.
CERVICAL CANCER SCREENING
After starting cervical cancer screening:
- Women ages 30 through 65 should be screened with either a Pap test every 3 years or the HPV test every 5 years or both tests every 5 years (called “cotesting”).
- Women who have been treated for precancer (cervical dysplasia) should continue to have Pap tests for 20 years after treatment or until age 65, whichever is longer.
If you have had your uterus and cervix removed (total hysterectomy), and you have not been diagnosed with cervical cancer or precancer (high grade cervcial neoplasia), you do not need cervical cancer screening.
CHOLESTEROL SCREENING
Cholesterol screening should begin at:
- Age 45 for women with no known risk factors for coronary heart disease
- Age 20 for women with known risk factors for coronary heart disease
Repeat cholesterol screening should take place:
- Every 5 years for women with normal cholesterol levels
- More often if changes occur in lifestyle (including weight gain and diet)
- More often if you have diabetes, heart disease, kidney problems, or certain other conditions
COLORECTAL CANCER SCREENING
If you are under age 45, talk to your provider about getting screened. You should be screened if you have a strong family history of colon cancer or polyps. Screening may also be considered if you have risk factors such as a history of inflammatory bowel disease or polyps.
If you are age 45 to 75, you should be screened for colorectal cancer. There are several screening tests available:
- A stool-based fecal occult blood (gFOBT) or fecal immunochemical test (FIT) every year
- A stool sDNA-FIT test every 1 to 3 years
- Flexible sigmoidoscopy every 5 years or every 10 years with stool testing with FIT done every year
- CT colonography (virtual colonoscopy) every 5 years
- Colonoscopy every 10 years
You may need a colonoscopy more often if you have risk factors for colorectal cancer, such as:
- Ulcerative colitis
- A personal or family history of colorectal cancer
- A history of growths in your colon called adenomatous polyps
DENTAL EXAM
- Go to the dentist once or twice every year for an exam and cleaning. Your dentist will evaluate if you have a need for more frequent visits.
DIABETES SCREENING
All adults who do not have risk factors for diabetes should be screened starting at age 35 and repeated every 3 years.
You should be tested more often if you have other risk factors for diabetes, such as:
- You a first-degree relative with diabetes
- You are overweight or have obesity, high blood pressure, prediabetes, or a history of heart disease
- If you are overweight and have other risk factors such as high blood pressure and are planning to become pregnant
EYE EXAM
- Have an eye exam every 2 to 4 years ages 40 to 54 and every 1 to 3 years ages 55 to 64. Your provider may recommend more frequent eye exams if you have vision problems or glaucoma risk.
- Have an eye exam that includes an examination of your retina (back of your eye) at least every year if you have diabetes.
IMMUNIZATIONS
Commonly needed vaccines include:
- Flu shot: get one every year.
- COVID-19 vaccine - ask your provider what is best for you
- Tetanus-diphtheria and acellular pertussis (Tdap) vaccine: have as one of your tetanus-diphtheria vaccines if you did not receive it as an adolescent.
- Tetanus-diphtheria: have a booster (or Tdap) every 10 years.
- Varicella vaccine: receive 2 doses if you never had chickenpox or the varicella vaccine and were born in 1980 or after.
- Hepatitis B vaccine: receive 2, 3, or 4 doses, depending on your exact circumstances, if you did not receive these as a child or adolescent, until age 59.
- Shingles (herpes zoster) vaccine: at or after age 50.
Ask your provider if you should receive other immunizations if you have certain health problems that increase your risk for some diseases such as pneumonia.
INFECTIOUS DISEASE SCREENING
Screening for hepatitis C:
- All adults ages 18 to 79 should get a one-time test for hepatitis C.
- Pregnant people should be screened at every pregnancy.
Screening for human immunodeficiency virus (HIV): all people ages 15 to 65 should get a one-time test.
Depending on your lifestyle and medical history, you may need to be screened for infections such as syphilis, chlamydia, and other infections.
LUNG CANCER SCREENING
You should have an annual screening for lung cancer with low-dose computed tomography (LDCT) if all of the following are present:
- You are age 50 to 80 years AND
- You have a 20 pack-year smoking history AND
- You currently smoke or have quit within the past 15 years
OSTEOPOROSIS SCREENING
If you are age 50 to 64 and have risk factors for osteoporosis, you should discuss screening with your provider.
Risk factors can include long-term steroid use, low body weight, smoking, heavy alcohol use, having a fracture after age 50, or a family history of hip fracture or osteoporosis.
PHYSICAL EXAM
All adults should visit their provider from time to time, even if they are healthy. The purpose of these visits is to:
- Screen for diseases
- Assess risk of future medical problems
- Encourage a healthy lifestyle
- Update vaccinations and other preventive care services
- Maintain a relationship with a provider in case of an illness
Your height, weight, and body mass index (BMI) should be checked at each exam.
During your exam, your provider may ask you about:
- Depression and anxiety
- Diet and exercise
- Alcohol and tobacco use
- Safety issues, such as using seat belts and smoke detectors and intimate partner violence
- Your medicines and risk for interactions
SKIN EXAM
- Your provider may check your skin for signs of skin cancer, especially if you're at high risk. People at high risk include those who have had skin cancer before, have close relatives with skin cancer, or have a weakened immune system.
References
Advisory Committee on Immunization Practices. Adult immunization scheduleby age. Recommendations for ages 19 years or older, United States, 2023.www.cdc.gov/vaccines/schedules/hcp/imz/adult.html. Updated April 27, 2023.Accessed July 30, 2023.
American Academy of Ophthalmology website. Comprehensive adult medical eyeexamination PPP 2020.www.aao.org/education/preferred-practice-pattern/comprehensive-adult-medical-eye-evaluation-ppp.Updated November 2020. Accessed July 30, 2023.
American Cancer Society website. Breast cancer early detection anddiagnosis: American Cancer Society recommendations for the early detection ofbreast cancer.www.cancer.org/cancer/breast-cancer/screening-tests-and-early-detection/american-cancer-society-recommendations-for-the-early-detection-of-breast-cancer.html.Updated January 14, 2022. Accessed July 30, 2023.
American College of Obstetricians and Gynecologists(ACOG) website. FAQ178: Mammography and other screening tests for breastproblems.www.acog.org/patient-resources/faqs/gynecologic-problems/mammography-and-other-screening-tests-for-breast-problems.Updated July 2022. Accessed July 30, 2023.
American College ofObstetricians and Gynecologists. FAQ163: Cervical cancer.www.acog.org/patient-resources/faqs/gynecologic-problems/cervical-cancer.Updated April 2021. Accessed July 30, 2023.American DentalAssociation website. Your top 9 questions about going to the dentist – answered!www.mouthhealthy.org/en/dental-care-concerns/questions-about-going-to-the-dentist.Accessed July 30, 2023.
American Diabetes AssociationProfessional Practice Committee. 2. Classification and Diagnosis of Diabetes:Standards of Medical Care in Diabetes-2023. Diabetes Care. 2023 Jan1;46(Suppl 1):S19-S30. PMID: 36507649. pubmed.ncbi.nlm.nih.gov/36507649/.
Atkins D, Barton M. The periodic health examination. In: Goldman L,Schafer AI, eds. Goldman-Cecil Medicine. 26th ed. Philadelphia, PA:Elsevier; 2020:chap 12.Brown HL, Warner JJ, Gianos E, et al; American Heart Association and theAmerican College of Obstetricians and Gynecologists. Promoting riskidentification and reduction of cardiovascular disease in women throughcollaboration with obstetricians and gynecologists: a presidential advisoryfrom the American Heart Association and the American College of Obstetriciansand Gynecologists. Circulation. 2018;137(24):e843-e852. PMID: 29748185pubmed.ncbi.nlm.nih.gov/29748185/.
Grundy SM, Stone NJ, Bailey AL, et al. 2018AHA/ACC/AACVPR/AAPA/ABC/ACPM/ADA/AGS/APhA/ASPC/NLA/PCNA Guideline on themanagement of blood cholesterol: a report of the American College ofCardiology/American Heart Association Task Force on Clinical PracticeGuidelines [published correction appears in J Am Coll Cardiol. 2019 Jun25;73(24):3237-3241]. J Am Coll Cardiol. 2019;73(24):e285-e350. PMID:30423393 pubmed.ncbi.nlm.nih.gov/30423393/.
Meschia JF, Bushnell C, Boden-Albala B; American Heart Association StrokeCouncil; et al. Guidelines for the primary prevention of stroke: a statementfor healthcare professionals from the American Heart Association/AmericanStroke Association. Stroke. 2014;45(12):3754-3832. PMID: 25355838pubmed.ncbi.nlm.nih.gov/25355838/.
Mora S, Libby P, Ridker PM. Primary prevention of cardiovascular disease.In: Libby P, Bonow RO, Mann DL, Tomaselli GF, Bhatt DL, Solomon SD, eds. Braunwald'sHeart Disease: A Textbook of Cardiovascular Medicine. 12th ed.Philadelphia, PA: Elsevier; 2022:chap 25.National Cancer Institute website. Breast cancer screening (PDQ) - healthprofessional version. www.cancer.gov/types/breast/hp/breast-screening-pdq.Updated June 7, 2023. Accessed July 30, 2023.
Studenski S, Van Swearingen J. Falls. In: Fillit HM, Rockwood K, Young J,eds. Brocklehurst's Textbook of Geriatric Medicine and Gerontology. 8thed. Philadelphia, PA: Elsevier; 2017:chap 103.US Preventive Services Task Force website. A and B recommendations.www.uspreventiveservicestaskforce.org/uspstf/recommendation-topics/uspstf-a-and-b-recommendations.Accessed July 30, 2023.
US Preventive Services Task Force website. Final recommendation statement.Breast cancer: Medication use to reduce risk.www.uspreventiveservicestaskforce.org/uspstf/recommendation/breast-cancer-medications-for-risk-reduction.Updated September 3, 2019. Accessed July 30, 2023.
US Preventive Services Task Force website. Final recommendation statement.Breast cancer: Screening.www.uspreventiveservicestaskforce.org/uspstf/recommendation/breast-cancer-screening.Updated January 11, 2016. Accessed July 30, 2023.
US Preventive Services Task Force website. Final recommendation statement.Cervical cancer: Screening.www.uspreventiveservicestaskforce.org/uspstf/recommendation/cervical-cancer-screening.Published August 21, 2018. Accessed July 30, 2023.
US Preventive Services Task Force website. Final recommendation statement.Colorectal cancer: Screening.www.uspreventiveservicestaskforce.org/uspstf/recommendation/colorectal-cancer-screening.Published May 18, 2021. Accessed July 30, 2023.
US Preventive Services Task Force website. Falls prevention in community-dwellingolder adults: Interventions. www.uspreventiveservicestaskforce.org/uspstf/recommendation/falls-prevention-in-older-adults-interventions.Published April 17, 2018. Accessed July 30, 2023.
US Preventive Services Task Force website. Final recommendation statement.Hepatitis C virus infection in adolescents and adults: Screening.www.uspreventiveservicestaskforce.org/uspstf/recommendation/hepatitis-c-screening.Published March 2, 2020. Accessed July 30, 2023.
US Preventive Services Task Force website. Final recommendation statement.Human immunodeficiency virus (HIV) infection: Screening.www.uspreventiveservicestaskforce.org/uspstf/recommendation/human-immunodeficiency-virus-hiv-infection-screening.Published June 11, 2019. Accessed July 30, 2023.
US Preventive Services Task Force website. Hypertension in adults:Screening.www.uspreventiveservicestaskforce.org/uspstf/recommendation/hypertension-in-adults-screening.Published April 27, 2021. Accessed July 30, 2023.
US Preventive Services Task Force website. Final recommendation statement:Lung cancer: Screening. www.uspreventiveservicestaskforce.org/uspstf/recommendation/lung-cancer-screening.Updated March 9, 2021. Accessed July 30, 2023.
US Preventive Services Task Force website. Final recommendation statement:Osteoporosis to prevent fractures: Screening. www.uspreventiveservicestaskforce.org/uspstf/recommendation/osteoporosis-screening.Updated June 26, 2018. Accessed July 30, 2023.
US Preventive Services Task Force website. Prediabetes and type 2diabetes: Screening.www.uspreventiveservicestaskforce.org/uspstf/recommendation/screening-for-prediabetes-and-type-2-diabetes.Updated August 24, 2021. Accessed July 30, 2023.
US Preventive Services Task Force website. Skin cancer: Screening.www.uspreventiveservicestaskforce.org/uspstf/recommendation/skin-cancer-screening.Updated April 18, 2023. Accessed July 30, 2023.
Whelton PK, Carey RM, Mancia G, Kreutz R, Bundy JD,Williams B. Harmonization of the American College of Cardiology/American HeartAssociation and European Society of Cardiology/European Society of HypertensionBlood Pressure/Hypertension Guidelines: Comparisons, Reflections, andRecommendations. Circulation. 2022;146:868–877. DOI:10.1161/CIRCULATIONAHA.121.054602.
Version Info
Last reviewed on: 4/30/2022
Reviewed by: David C. Dugdale, III, MD, Professor of Medicine, Division of General Medicine, Department of Medicine, University of Washington School of Medicine. Also reviewed by David Zieve, MD, MHA, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team. Editorial update 04/18/2023. Internal review and update on 08/01/23.
