What is a Meningioma?
Meningiomas represent about a third of all primary brain tumors. Often benign, they tend to affect men and women between the ages of 40 and 70; they are extremely rare in children. They affect women more often than men.
These tumors arise from the meninges, which are the membranes around the brain and spinal cord. While meningioma cell growth is uncontrolled, it usually is not malignant (cancerous). Meningiomas are unlikely to spread to other parts of the body (metastasis). At Mount Sinai, we have extensive experience diagnosing and treating meningiomas.
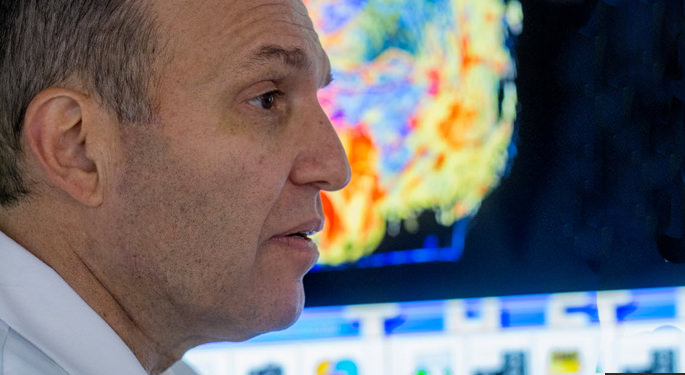
"Benign tumors, which seem to strike out of the blue, can cause a range of problems, but they are treatable," says Joshua Bederson, MD, Professor and Chair of Neurosurgery at The Mount Sinai Health System. "The initial diagnosis is often terrifying, but it's important to keep in mind that we can get our patients through this."
If you leave a meningioma untreated, it can grow as large as a grapefruit can cause persistent headaches, nausea, loss of neurological function, weakness and/or numbness and tingling on one side of the body, seizures, hearing or vision loss, balance problems, and muscle weakness. The symptoms of a meningioma depend on its size and location. A small tumor pressing on the optic nerve can cause visual loss while a tumor located in the convexity, or on the surface of the brain, can be quite large before you notice any symptoms.
We do not know what causes meningiomas, according to the American Brain Tumor Association, though certain factors can increase your risk. These factors include prior radiation to the head, having a genetic condition called neurofibromatosis type 2, and having had breast cancer.
We do not know how to prevent meningiomas. Recognizing the symptoms is important and early detection allows for more treatment options before the tumor gets too large.
Diagnostics
To correctly diagnose a meningioma, we first conduct a neurological exam to see if any of these symptoms are present. The neurologist or neurosurgeon may request one or more of these non-invasive brain scans to better diagnose the tumor and to see detailed images:
- Magnetic resonance imaging scans use magnetic waves to allow doctors to see two- and three-dimensional pictures of the brain and spine. The machine uses a magnet, radio waves, a computer, and occasionally a contrast dye injected into the patient to create the detailed pictures.
- Computed tomography scans are a type of X-ray that we use to see two–dimensional pictures of the brain and spine. We can use contrast dye to help distinguish tumors from other structures in the brain.
With that information, our team will determine the best possible treatment option for each patient.
Meningioma Grading
The World Health Organization classifies meningiomas from grade I to III based on location, type, and histology. Using a three-tier grading system, our team of doctors examines your tumor’s tissue and assigns it a grade, after being evaluated by a neuropathologist. This grade helps us determine the treatment plan.
- Grade I is the most common and accounts for 90 percent of all meningiomas. These meningiomas are benign and usually do not produce symptoms. We monitor them closely.
- Grade II meningiomas, or atypical meningiomas, usually grow more rapidly than benign ones and have a greater chance of growing back.
- Grade III is the most aggressive type of meningioma and are typically malignant. Grade III meningiomas are the most aggressive and fastest growing type. They also recur more often than lower-graded meningiomas. Relatively rare, Grade III meningiomas account for only about 2 percent of meningiomas. Men with Grade III meningiomas are more likely to have a high rate of cell division, also known as mitosis, than women, and these tumors can spread to other locations. Typically, we remove these tumors completely and follow surgery with radiation treatment.