New Signaling Role for Key Protein May Contribute to Wound Healing, Tumor Growth and Inflammatory Diseases
A key protein may represent a new way to use the immune system to speed healing and counter inflammatory, infectious and autoimmune diseases, according to study led by researchers at the Icahn School of Medicine at Mount Sinai and published in the December issue of Cell Reports.
The current study results revolve around proteinases, enzymes that break down proteins as part of cellular life. Matrix metalloproteinases or MMPs specifically target the extracellular matrix, the non-cell, structural framework within tissues. Beyond that role, the new study found that one member of this family, MMP-2, has another signaling role related to the human immune system. It may shift a set of cells to become part of immune response that accelerates healing in some cases, but may worsen inflammatory disease in others.
Drug designers may be able to leverage the newfound MM-2 mechanisms to prevent the contribution of inflammatory signals to tumor growth and autoimmune diseases, or to promote wound healing.
“Our results show that MMP-2 uses a multitude of mechanisms to modulate the immune system,” says the study’s lead investigator Nina Bhardwaj, MD, PhD, Director of Immunotherapy, Tisch Cancer Center at Mount Sinai, Professor of Medicine, Hematology and Oncology, Icahn School of Medicine at Mount Sinai. “These data provides context to how this mechanism happens and could lead to novel treatments.”
The backdrop for the study finding is the body’s initial, vague reaction to any invading organism expands into a precise and massive counterattack. That expansion starts when a dendritic cell “swallows” a piece of any invader encountered, ferries it to the nearest lymph node and presents it there for notice by lymphocytes (B cells and T cells), the workhorses of the immune system. DCs exposed to MMP-2 send signals that change gene expression such that more of a protein called OX40L is made, according to the study authors. OX40L is a signaling protein that links into a receptor protein on the surface of dendritic cells, like a key fitting into a lock, with their interaction changing the shape of the receptor such that other signals get sent. Among these is one that causes more immune cells within a certain part of the immune system, TH2 cells, to be made.
Though vital to effective immune responses to worms, Th2 cells have a dark side, in some cases triggering B cells to produce antibodies that recognize the body’s own cells as foreign and that destroy the kidneys of lupus patients and the joints of patients with rheumatoid arthritis. Shifting T cells in the Th2 path generally encourages inflammation.
If MMP-2 signaling leads to the presence of more Th2 T cells, it means Th2 cells will secrete more inflammatory TH2 cytokines like TNF-alpha, and interleukins 4 and 13, which fight parasite infections, but that can also contribute to autoimmune diseases if present in too large amounts. MMP-2 is also over-expressed in tumors, where it promotes cancer progression. This may in part be due to its ability to skew T cells toward Th2 differentiation, a process called type-2 polarization.
Th2 cells also contribute to wound healing because they produce cytokines, which fight infection and ultimately repair tissue. The tissue repair functions of MMP-2‘s may be due to the ability to drive Th2 immune response.
“MMP-2-mediated signaling either through direct injection or through mimics could promote wound healing but these proposed functions will require further investigation in disease-specific models,” says Dr. Bhardwaj. “Further discovery of new MMP-2 functions could lead to new reagents of inflammatory responses.”
The work was supported by a research grant from the National Institute of Health and a CLIP Award from the Cancer Research Institute. Researchers from Rockefeller University, Stanford University, New York University, Emory University and the Institut National de la Sante et de la Recherhe Medicale (INSERM) in Paris contributed to the study.
About the Mount Sinai Health System
Mount Sinai Health System is one of the largest academic medical systems in the New York metro area, with more than 43,000 employees working across eight hospitals, over 400 outpatient practices, nearly 300 labs, a school of nursing, and a leading school of medicine and graduate education. Mount Sinai advances health for all people, everywhere, by taking on the most complex health care challenges of our time — discovering and applying new scientific learning and knowledge; developing safer, more effective treatments; educating the next generation of medical leaders and innovators; and supporting local communities by delivering high-quality care to all who need it.
Through the integration of its hospitals, labs, and schools, Mount Sinai offers comprehensive health care solutions from birth through geriatrics, leveraging innovative approaches such as artificial intelligence and informatics while keeping patients’ medical and emotional needs at the center of all treatment. The Health System includes approximately 7,300 primary and specialty care physicians; 13 joint-venture outpatient surgery centers throughout the five boroughs of New York City, Westchester, Long Island, and Florida; and more than 30 affiliated community health centers. We are consistently ranked by U.S. News & World Report's Best Hospitals, receiving high "Honor Roll" status, and are highly ranked: No. 1 in Geriatrics and top 20 in Cardiology/Heart Surgery, Diabetes/Endocrinology, Gastroenterology/GI Surgery, Neurology/Neurosurgery, Orthopedics, Pulmonology/Lung Surgery, Rehabilitation, and Urology. New York Eye and Ear Infirmary of Mount Sinai is ranked No. 12 in Ophthalmology. U.S. News & World Report’s “Best Children’s Hospitals” ranks Mount Sinai Kravis Children's Hospital among the country’s best in several pediatric specialties.
For more information, visit https://www.mountsinai.org or find Mount Sinai on Facebook, Twitter and YouTube.
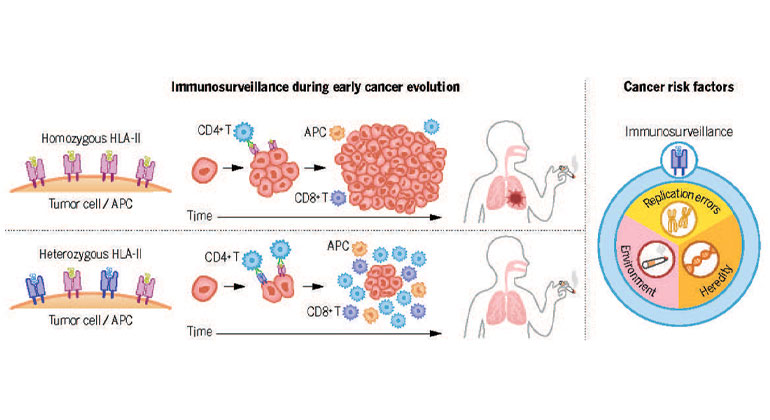
Study Reveals New Insights Into Immune System Role in Lung Cancer Risk
Feb 22, 2024 View All Press Releases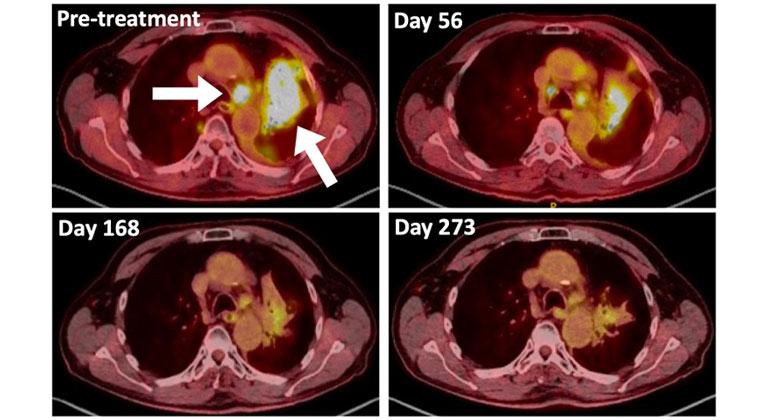
A Type of Allergy Medicine Might Help Treat Lung Cancer, Research Suggests
Dec 06, 2023 View All Press ReleasesMount Sinai’s Staten Island Cancer Center Moves to New Site
Nov 09, 2023 View All Press Releases
Diabetes May Accelerate Blood Cancer Growth, Yet Survival Outcomes Differ by Race
Sep 29, 2023 View All Press Releases
Mount Sinai Awarded $3.4 Million to Study Prostate Cancer in People With HIV
Sep 12, 2023 View All Press Releases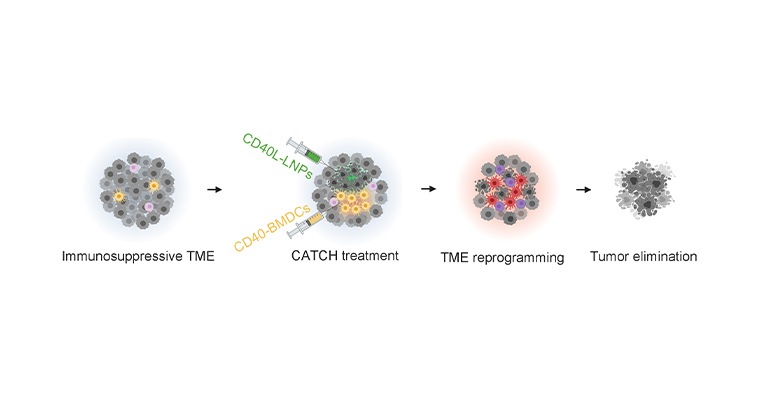
New RNA-based Therapy Combats Melanoma in Mouse Models
Jul 27, 2023 View All Press Releases

