The Mount Sinai Hospital Experts Debunk the 5 Most Common Postpartum Depression Myths Plaguing Latina Moms
Postpartum depression is the #1 complication of pregnancy among Latinas.
New York, NY, May 2, 2012 – According to a recent study, more than 30% of Latinas in the U.S. and Mexico suffer perinatal or postpartum depression, making it the number one complication of pregnancy among Latinas. In an effort to raise visibility for a disease that is often dismissed, physicians from The Mount Sinai Hospital debunked the 5 most prevalent Latino myths about postpartum depression, a type of depression that affects some women after childbirth. A growing and significant audience, Hispanic Mothers accounted for approximately 24% of births nationwide and 24% in New York State. Lack of awareness, understanding and acceptance of the disease has resulted in powerful myths impacting the lives of women who are experiencing one of life’s most joyous events, especially in the Latino home.
Myth # 1 – “I feel so bad. Shouldn't I be happy about my newborn? Maybe I am not a good mother.”
False. It is not uncommon for women to experience temporary mood disorders or "blues" after giving birth. According to Kim Klipstein, MD, Director of Behavioral Medicine and Consultation Psychiatry at The Mount Sinai Hospital, “postpartum depression is different than "baby blues," which is a mild form of depression that occurs within a few days after childbirth and lasts up to a week.” Conversely, Dr. Klipstein added, “postpartum depression typically emerges over the first 2-3 months after childbirth but may occur at any point during the first year after delivery. Symptoms may include: loss of interest or pleasure in life, loss of appetite, rapid mood swings, fear of hurting or killing oneself or one's child. These feelings can disrupt a woman's ability to function on a daily basis and make bonding with the newborn difficult. More serious symptoms associated with postpartum depression that require immediate medical attention include: lack of interest in your infant, suicidal thoughts or thoughts of harming your baby, hallucinations or delusions.”
Myth # 2 – “My Mother says that postpartum depression has not affected the women in our family. If I speak up, they’ll think I’m crazy!"False. Although, for many Latinos, mental illness is considered shameful – a topic that shouldn't be discussed, do not let misinformation, uncertainty or shame get in the way of you getting the help you need. In Latino cultures, which have deep-rooted family values and high expectations of new moms, Hispanic women reject feelings of unhappiness during pregnancy and after the baby are born. If their own mothers never expressed negative feelings about pregnancy, they believe they must follow her example. But keep in mind that postpartum depression is a real illness and, if left untreated, it can interfere with mother-child bonding and lead to serious long term problems. According to Dr. Klipstein of The Mount Sinai Hospital, “children of mothers who have untreated postpartum depression are more likely to have behavioral problems, such as sleeping and eating difficulties, temper tantrums and hyperactivity.” Dr. Klipstein concludes, “delays in language development are more common as well.”
Myth # 3 – “Because of my age, I am at higher risk of experiencing postpartum depression.”
False. Postpartum depression can affect any woman of childbearing age regardless of socio-economic status, education level, racial and ethnic background and age. According to Dr. Klipstein of The Mount Sinai Hospital, “the cause of postpartum depression is unclear. It may be related to sudden hormonal changes during and after delivery. Untreated thyroid conditions may also be associated with postpartum depression.” Some factors that increase your chances of developing postpartum depression include: a previous episode of depression, lack of support system and/or a strained relationship with your partner, a history of an anxiety disorder, depression during pregnancy, and a family history of depression. Feeling overwhelmed and anxious are normal feelings for any mother, but if they begin to interfere with your ability to care for yourself and your baby it could signal something more serious and it is important to seek help.
Myth # 4 – “Postpartum depression cannot be prevented. I just need to get through it.”
False. Aside from the biological changes, a variety of physical, psychological, and environmental factors can lead to postpartum depression. The good news is that the disease is treatable and should be addressed immediately. According to Dr. Kim Klipstein of The Mount Sinai Hospital, “by identifying your risk factors and understanding postpartum stress, you can anticipate a plan with your doctor.” And, upon returning from the hospital after child delivery, Dr. Klipstein suggests that “Mothers follow a sensible diet, eliminating alcohol and caffeine; limit visitors; let family and friends know how they can be of help; have a solid support system and get sufficient rest.”
Myth # 5 – “I would rather just put up with the postpartum depression, than be prescribed medications that will affect my breast milk and harm my baby.”
False. Women should talk to their doctors as soon as they experience any of the symptoms of postpartum depression to determine the most suitable treatment and not make any assumptions. According to Dr. Kim Klipstein of The Mount Sinai Hospital, “treatment for postpartum depression may include counseling, medication, or both.” Though there may be risks associated with taking medication while breastfeeding, there are ways to minimize this risk and there are also equal risks associated with not treating depression during this time period. Risks and benefits of treatment should be discussed in detail with a health care professional so that the best treatment option for you and your baby can be mutually decided upon.
If you have experienced any of the symptoms of postpartum depression or, if you need help determining whether you, a family member or friend has the disease, contact your doctor immediately. Seeking treatment will afford you the opportunity to feel better and enjoy one of the happiest periods in a woman’s life. For an appointment with a specialist contact: 1-877-241-4983 or visit www.mountsinai.org/Latino
###
About The Mount Sinai Medical Center
The Mount Sinai Medical Center encompasses both The Mount Sinai Hospital and Mount Sinai School of Medicine. Established in 1968, Mount Sinai School of Medicine is one of the leading medical schools in the United States. The Medical School is noted for innovation in education, biomedical research, clinical care delivery, and local and global community service. It has more than 3,400 faculty in 32 departments and 14 research institutes, and ranks among the top 20 medical schools both in National Institutes of Health (NIH) funding and by U.S. News & World Report.
The Mount Sinai Hospital, founded in 1852, is a 1,171-bed tertiary- and quaternary-care teaching facility and one of the nation’s oldest, largest and most-respected voluntary hospitals. In 2011, U.S. News & World Report ranked The Mount Sinai Hospital 16th on its elite Honor Roll of the nation’s top hospitals based on reputation, safety, and other patient-care factors. Of the top 20 hospitals in the United States, Mount Sinai is one of 12 integrated academic medical centers whose medical school ranks among the top 20 in NIH funding and US News & World Report and whose hospital is on the US News & World Report Honor Roll. Nearly 60,000 people were treated at Mount Sinai as inpatients last year, and approximately 560,000 outpatient visits took place.
For more information, visit www.mountsinai.org/Latino Follow us on Twitter @mountsinainyc.
Contact:
Andrés Reyes, Latin2Latin Marketing + Communications.
954 376 4800 / andres@latin2latin.com
About the Mount Sinai Health System
Mount Sinai Health System is one of the largest academic medical systems in the New York metro area, with more than 43,000 employees working across eight hospitals, over 400 outpatient practices, nearly 300 labs, a school of nursing, and a leading school of medicine and graduate education. Mount Sinai advances health for all people, everywhere, by taking on the most complex health care challenges of our time — discovering and applying new scientific learning and knowledge; developing safer, more effective treatments; educating the next generation of medical leaders and innovators; and supporting local communities by delivering high-quality care to all who need it.
Through the integration of its hospitals, labs, and schools, Mount Sinai offers comprehensive health care solutions from birth through geriatrics, leveraging innovative approaches such as artificial intelligence and informatics while keeping patients’ medical and emotional needs at the center of all treatment. The Health System includes approximately 7,300 primary and specialty care physicians; 13 joint-venture outpatient surgery centers throughout the five boroughs of New York City, Westchester, Long Island, and Florida; and more than 30 affiliated community health centers. We are consistently ranked by U.S. News & World Report's Best Hospitals, receiving high "Honor Roll" status, and are highly ranked: No. 1 in Geriatrics and top 20 in Cardiology/Heart Surgery, Diabetes/Endocrinology, Gastroenterology/GI Surgery, Neurology/Neurosurgery, Orthopedics, Pulmonology/Lung Surgery, Rehabilitation, and Urology. New York Eye and Ear Infirmary of Mount Sinai is ranked No. 12 in Ophthalmology. U.S. News & World Report’s “Best Children’s Hospitals” ranks Mount Sinai Kravis Children's Hospital among the country’s best in several pediatric specialties.
For more information, visit https://www.mountsinai.org or find Mount Sinai on Facebook, Twitter and YouTube.
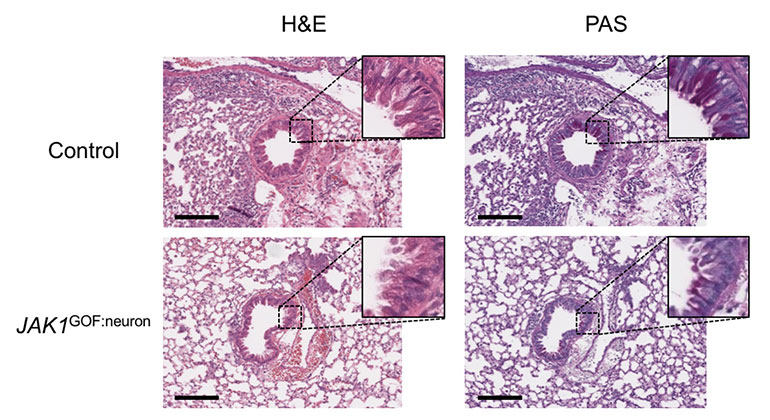
New Insights Revealed On Tissue-Dependent Roles of JAK Signaling in Inflammation
Dec 21, 2023 View All Press Releases